Trombophilia
neuroophthalmological manifestation
DOI:
https://doi.org/10.70313/2718.7446.v16.n03.248Keywords:
thrombophilia, papilledema, cerebral venous sinus thrombosis, intracanial hypertension, thrombogenesis, neurooftalmologyAbstract
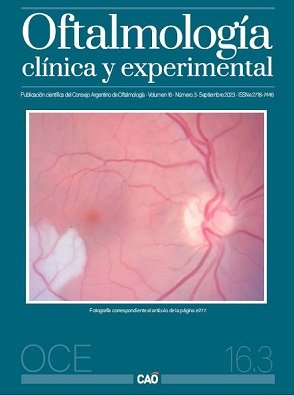
Objective: Report on a form of thrombophilia from the clinical case of a patient with papilledema caused by 2 cerebral venous sinus thrombosis, product of such disease.
Case report: 47-year-old female patient who presented to the ophthalmology ER reporting episodes of transient darkening of vision, severe headache and tinnitus. During the ophthalmologic examination she had evidence of bilateral papilledema, showing cerebral venous sinus thrombosis during the magnetic resonance angiography as a first instance pathophysiological factor. After thourough clinical and lab exams, thrombophilia diagnosis is confirmed as the cause for the cerebral venous sinus thrombosis, and so she was treated with anticoagulants showing a remarkable improvement in the clinical scenario.
Conclusion: This case highlights that thrombophilia can be a cause of cerebral venous sinus thrombosis, also causing bilateral papilledema.
Downloads
References
Saposnik G, Barinagarrementeria F, Brown RD Jr et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42: 1158-1192.
Medicherla CB, Pauley RA, de Havenon A et al. Cerebral venous sinus thrombosis in the Covid-19 pandemic. J Neuroophthalmol 2020; 40: 457-462.
Ferro JM, Canhão P, Stam J et al. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study of Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004; 35: 664-670.
Duman T, Uluduz D, Midi I, VENOST Study Group et al. A multicenter study of 1144 patients with cerebral venous thrombosis: the VENOST study. J Stroke Cerebrovasc Dis 2017; 26: 1848–1857.
Aaron S, Arthur A, Prabakhar AT, et al. Spectrum of visual impairment in cerebral venous thrombosis: importance of tailoring therapies based on pathophysiology. Ann Indian Acad Neurol 2017; 20: 294-301.
Altuna D, Ceresetto J, Fassi D et al. Trombofilias. Buenos Aires: Sociedad Argentina de Hematología, 2012, p. 471-481. Disponible en: http://www.sah.org.ar/docs/471-481.12.SAH_GUIA2012_Trombofilia.pdf
Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology 2002; 59:1492-1495.
Linn J, Brückmann H. Cerebral venous and dural sinus thrombosis: state-of-the-art imaging. Clin Neuroradiol 2010; 20: 25-37.
Brune AJ, Girgla T, Trobe JD. Complications of ventriculoperitoneal shunt for idiopathic intracranial hypertension: a single-institution study of 32 patients. J Neuroophthalmol 2021; 41: 224-232.
Downloads
Published
Issue
Section
License
Copyright (c) 2023 Consejo Argentino de Oftalmología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Con esta licencia no se permite un uso comercial de la obra original, ni la generación de obras derivadas. Las licencias Creative Commons permiten a los autores compartir y liberar sus obras en forma legal y segura.