Mycoplasma induced mucositis and rash (MIRM)
case report
DOI:
https://doi.org/10.70313/2718.7446.v18.n2.413Keywords:
MIRM, mycoplasma-induced rash and mucositis, Stevens-Johnson syndrome, toxic epidermal necrolysis, bilateral conjunctivitis, mucositis, antibiotic therapy, corticotherapyAbstract
Objective. Mycoplasma Pneumoniae has been reported as a causative agent of respiratory disease with mucosal involvement, including ocular mucosa, which has been termed “Mycoplasma-induced Mucositis and Rash (MIRM)”. Although it has a similar presentation and manifestations, it should be differentiated from conditions such as Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN) or Erythema Multiforme (EM), since the treatment and evolution will be different. Our aim is to present the case of a male patient with MIRM.
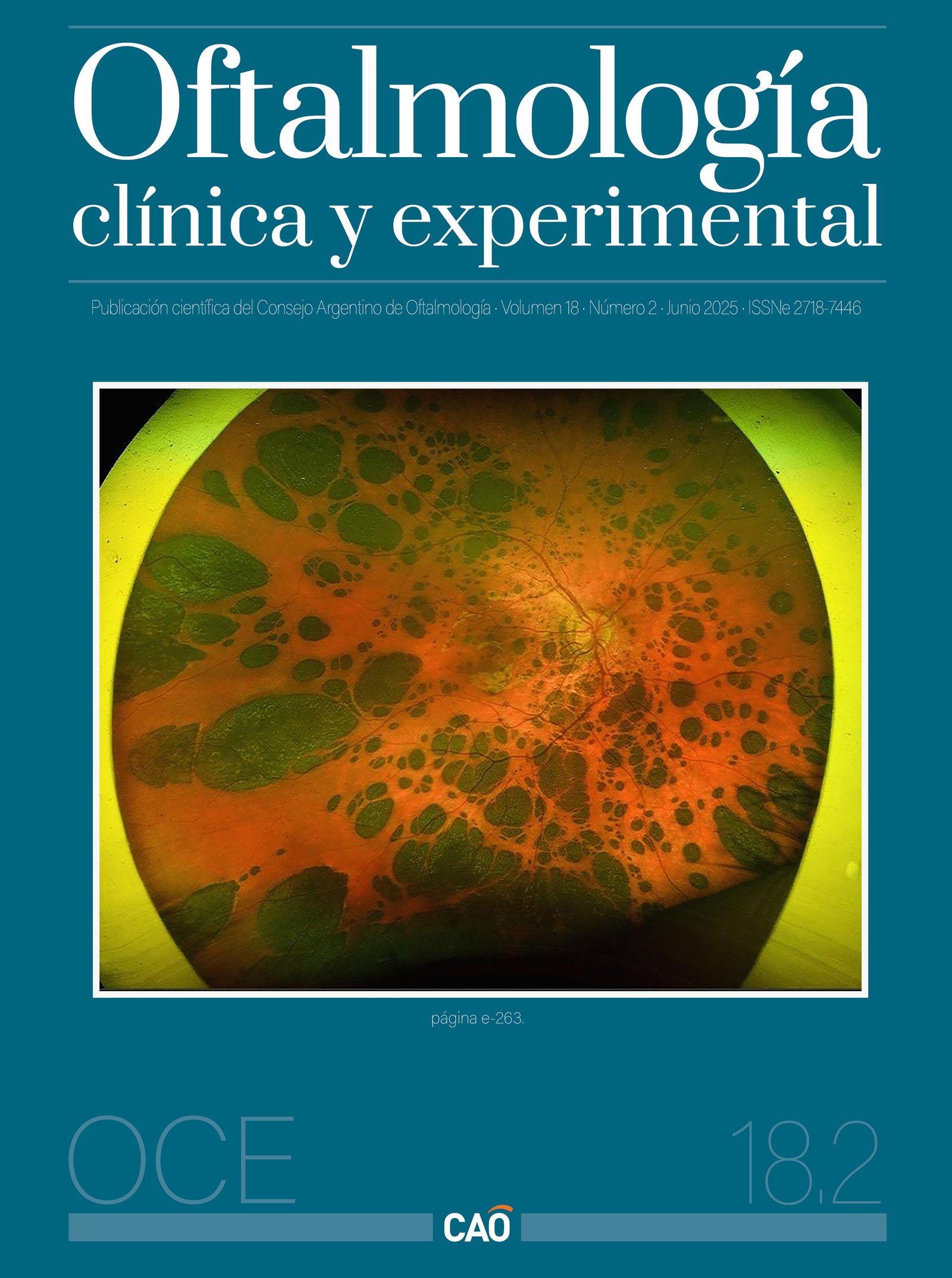
Case report A 21-year-old male with mucocutaneous systemic involvement and respiratory symptoms was referred to ophthalmology for bilateral ocular pain. In the anamnesis he reported fever, odynophagia, oral and ocular lesions, dyspnea and hemoptysis. Physical examination revealed extensive ulcers in oral mucosa and conjunctivitis with anterior scleritis. Imaging studies showed pulmonary infiltrates compatible with infectious process, and multiple common infectious etiologies were ruled out. Suspected MIRM (Mycoplasma-Induced Rash and Mucositis), specific antibodies were requested, with highly positive results for Mycoplasma pneumoniae. Treatment was started with ceftriaxone, clarithromycin and intravenous methylprednisolone, in addition to topical ocular therapy.
The patient evolved favorably with no respiratory, oral or ophthalmologic sequelae after 7 days, and was discharged with outpatient follow-up.
Conclusion. The case presented exemplifies the clinical manifestation of MIRM, pointing out the keys to establish a timely diagnosis and an adequate therapeutic intervention, as it happened with our patient through a multidisciplinary approach
Downloads
References
1. Alawad S, Alsaeed N, Burnette B, Colantonio M, Kasson L. Reactive infectious mucocutaneous eruption (RIME) in an adult male with Mycoplasma pneumoniae: a case report. Cureus 2025; 17(1): e78301. doi:10.7759/cureus.78301.
2. Miyashita N, Nakamori Y, Ogata M et al. Clinical differences between community-acquired Mycoplasma pneumonia pneumonia and COVID-19 pneumonia. J Clin Med 2022; 11(4): 964. doi:10.3390/jcm11040964.
3. Biagi C, Cavallo A, Rocca A et al. Pulmonary and extrapulmonary manifestations in hospitalized children with mycoplasma pneumoniae infection. Microorganisms 2021; 9(12): 2553. doi:10.3390/microorganisms9122553.
4. Lofgren D, Lenkeit C. Mycoplasma pneumoniae-induced rash and mucositis: a systematic review of the literature. Spartan Med Res J 2021; 6(2): 25284. doi:10.51894/001c.25284.
5. Villarroel J, Bustamante MC, Denegri M, Pérez L. Manifestaciones muco-cutáneas de la infección por Mycoplasma pneumoniae: presentación de cuatro casos. Rev Chilena Infectol 2009; 26(5): 457-463.
6. Gise R, Elhusseiny AM, Scelfo C, Mantagos IS. Mycoplasma pneumoniae-induced rash and mucositis: a longitudinal perspective and proposed management criteria. Am J Ophthalmol 2020; 219: 351-356. doi:10.1016/j.ajo.2020.06.010.
7. Martínez-Pérez M, Imbernón-Moya A, Lobato-Berezo A, Churruca-Grijelmo M. Exantema mucocutáneo inducido por Mycoplasma pneumoniae: ¿un nuevo síndrome separado del eritema multiforme? Un nuevo caso y revisión de la literatura. Actas Dermosifiliogr 2016; 107(7): e47-e51. doi:10.1016/j.ad.2015.09.023.
8. Guzmán Tenaa P, Rodríguez Ramosa M, Lloret Ruizb C, Vázquez Álvarez ML. Erupción mucocutánea infecciosa reactiva (RIME): expandiendo el espectro de los exantemas mucocutáneos. Actas Dermosifiliogr 2024; 115(10): 1097-1099. doi: 10.1016/j.ad.2023.02.038.
9. Canavan TN, Mathes EF, Frieden I, Shinkai K. Mycoplasma pneumoniae-induced rash and mucositis as a syndrome distinct from Stevens-Johnson syndrome and erythema multiforme: a systematic review. J Am Acad Dermatol 2015; 72(2): 239-245. doi:10.1016/j.jaad.2014.06.026.
10. Haseeb A, Elhusseiny AM, ElSheikh RH, Tahboub MA, Kwan JT, Saeed HN. Ocular involvement in Mycoplasma induced rash and mucositis: a systematic review of the literature. Ocul Surf 2023; 28: 1-10. doi:10.1016/j.jtos.2022.11.007.
11. De Andrés B, Tejeda V, Arrozpide L. Mucositis por Mycoplasma: un caso clínico que apoya su diferenciación del síndrome de Stevens Johnson. Med Cutan Iber Lat Am 2017; 45(3): 224-227.
12. De Luigi G, Meoli M, Zgraggen L et al. Mucosal respiratory syndrome: a systematic literature review. Dermatology 2022; 238(1): 53-59. doi:10.1159/000514815.
13. Gandelman JS, Kim EY, Grzegorczyk AM, Zejnullahu K, Edson RS. Mycoplasma pneumoniae-induced rash and mucositis in a previously healthy man: a case report and brief review of the literature. Open Forum Infect Dis 2020; 7(10): ofaa437. doi:10.1093/ofid/ofaa437.
14. Smilga AS, Fournier S, Veillette H, Légaré MÈ, Gilbert M. A rare case of Mycoplasma-induced rash and mucositis in a 44-year-old female patient. JAAD Case Rep 2020; 6(12): 1333-1335. doi:10.1016/j.jdcr.2020.09.014 [Errata corregida en: JAAD Case Rep. 2021; 8:63. doi:10.1016/j.jdcr.2021.01.003].
15. Gonçalves R, Gata L, Brett A. Mycoplasma pneumoniae-associated mucositis. BMJ Case Rep 2021; 14(4): e239086. doi:10.1136/bcr-2020-239086.
16. Zão I, Ribeiro F, Rocha V, Neto P, Matias C, Jesus G. Mycoplasma pneumoniae-associated mucositis: a recently described entity. Eur J Case Rep Intern Med 2018; 5(11): 000977. doi:10.12890/2018_000977.
17. Berzosa-López R, Carro-Rodríguez MA, de la Parte-Cancho M et al. Las mil y una caras del Mycoplasma. Pediatría Atención Primaria 2021; 23(91): 297-299.
18. Jin HD, Siatkowski RM, Siatkowski RL. Ocular manifestations of mycoplasma-induced rash and mucositis. J AAPOS 2020; 24(4): 249-251. doi:10.1016/j.jaapos.2020.04.006.
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Consejo Argentino de Oftalmología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Con esta licencia no se permite un uso comercial de la obra original, ni la generación de obras derivadas. Las licencias Creative Commons permiten a los autores compartir y liberar sus obras en forma legal y segura.