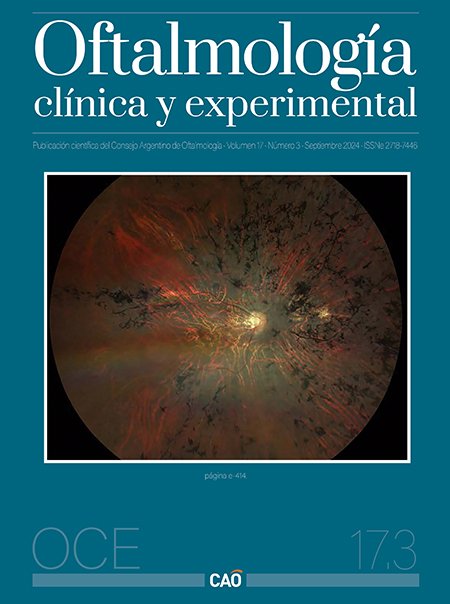
ROP management protocol in extreme regions
an eleven-year retrospective study in Rio Grande, Tierra del Fuego
DOI:
https://doi.org/10.70313/2718.7446.v17.n03.345Keywords:
retinopathy of prematurity, ROP, remote regions, ROP protocols, ROP epidemiology, South-AmericaAbstract
Objective: To review the long-term performance of a protocol for the management of retinopathy of prematurity (ROP) in Río Grande, Tierra del Fuego, and to discuss similarities and differences with other places with similar environmental characteristics.
Materials and methods: Retrospective study in which the medical records of patients born prematurely between 2013 and 2024 at the Regional Hospital of Río Grande and a private clinic in the same city were reviewed. The number of patients with ROP, the management performed and its outcome were evaluated, implementing a protocol of care that considered the limitations of the region, both climatic, geographical and accessibility.
Results: We found 378 medical records of premature infants, where 6 cases developed ROP (prevalence of 1.6%) in the span of 11 years. All were treated on the island, without the need for referral, with the assistance of a specialist from the city of Buenos Aires, who performed laser treatment together with the local physician, who
followed them up. Follow-up in the 6 cases was between 1 to 6 years and no infant had ROP evolution, retinal detachment, with no cases of low vision or blindness.
Conclusion: The cases of ROP treated with the present protocol by this medical team, throughout eleven years in Rio Grande, evolved favorably, without finding cases of
blindness.
Downloads
References
Padeken D, Sotiriou D, Boddy K, Gerzer R. Health care in remote areas. J Med Syst 1995; 19: 69-76.
Watanabe M, Risi R, Tafuri MA et al. Bone density and genomic analysis unfold cold adaptation mechanisms of ancient inhabitants of Tierra del Fuego. Sci Rep 2021; 11: 23290.
Blencowe H, Lawn JE, Vazquez T et al. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatr Res 2013; 74 (Suppl 1): 35-49.
Dammann O, Hartnett ME, Stahl A. Retinopathy of prematurity. Dev Med Child Neurol 2023; 65: 625-631.
Fevereiro-Martins M, Marques-Neves C, Guimarães H, Bicho M. Retinopathy of prematurity: a review of pathophysiology and signaling pathways. Surv Ophthalmol 2023; 68: 175-210.
Argentina. Ministerio de Salud. Grupo ROP Argentina. Guía de práctica clínica para la prevención, diagnóstico y tratamiento de la retinopatía del prematuro (ROP). Buenos Aires: Ministerio de Salud, 2017.
Zárate RG, Bebiglia A, Mansilla C et al. Retinopatía del prematuro en Río Grande, Tierra del Fuego, Argentina. Oftalmol Clin Exp 2022; 15: e405-e411.
Alda E, Lomuto CC, Benítez AM et al. Results of the National Program for the Prevention of Blindness in Childhood by Retinopathy of Prematurity in Argentina (2004-2016). Arch Argent Pediatr 2018; 116: 386-393.
Chen J, Zhu Y, Li L et al. Visual impairment burden in retinopathy of prematurity: trends, inequalities, and improvement gaps. Eur J Pediatr 2024; 183: 1891-1900.
Chiang MF, Quinn GE, Fielder AR et al. International classification of retinopathy of prematurity, third edition. Ophthalmology 2021; 128: e51-e68.
Pérez Lapponi V. Retinopatía del prematuro en cuatro centros neonatológicos de la provincia de Buenos Aires. Oftalmol Clin Exp 2020; 13: 32-40.
Fondo de las Naciones Unidas para la Infancia (UNICEF). Derechos de los recién nacidos prematuros. Derecho 6: derecho a la prevención de la ceguera por retinopatía del prematuro (ROP). Argentina, 2014.
Argentina. Ministerio de Salud. Dirección de Maternidad e Infancia. Grupo de Trabajo Colaborativo Multicéntrico: Prevención de la Ceguera en la Infancia por Retinopatía del Prematuro (ROP). Epidemiología de la retinopatía del prematuro en servicios públicos de la Argentina durante 2008. Oftalmol Clin Exp 2010; 3: 130-135.
Sabri K, Ells AL, Lee EY et al. Retinopathy of prematurity: a global perspective and recent developments. Pediatrics 2022; 150: e2021053924.
Quinn GE, Vinekar A. The role of retinal photography and telemedicine in ROP screening. Semin Perinatol 2019; 43: 367-374.
Brady CJ, D’Amico S, Campbell JP. Telemedicine for retinopathy of prematurity. Telemed J E Health 2020; 26: 556-564.
Young BK, Cole ED, Shah PK et al. Efficacy of smartphone-based telescreening for retinopathy of prematurity with and without artificial intelligence in India. JAMA Ophthalmol 2023; 141: 582-588.
Coyner AS, Murickan T, Oh MA et al. Multinational external validation of autonomous retinopathy of prematurity screening. JAMA Ophthalmol 2024; 142: 327-335.
Kirby RP, Malik ANJ, TPP Survey and Meeting Participants Collaborator Group et al. Improved screening of retinopathy of prematurity (ROP): development of a target product profile (TPP) for resource-limited settings. BMJ Open Ophthalmol 2023; 8:
e001197.
Subramaniam A, Orge F, Douglass M et al. Image harmonization and deep learning automated classification of plus disease in retinopathy of prematurity. J Med Imaging (Bellingham) 2023; 10: 061107.
Saidman GR, Monteoliva F, Urrets-Zavalía JA. Headband-mounted holder for hands-free indirect fundoscopy through a smartphone. Invest Ophthalmol Vis Sci 2016; 57: 6294.
Sankar MJ, Sankar J, Chandra P. Anti-vascular endothelial growth factor (VEGF) drugs for treatment of retinopathy of prematurity. Cochrane Database Syst Rev 2018; 1: CD009734.
Consenso sobre el uso de Avastin® para el tratamiento de la retinopatía del prematuro en la Argentina. Oftalmol Clin Exp 2023; 16 (Sup. 1): eS1-eS20. Disponible en: https://revistaoce.com/index.php/revista/issue/view/18
Hartnett ME, Stahl A. Laser versus anti-VEGF: a paradigm shift for treatment-warranted retinopathy of prematurity. Ophthalmol Ther 2023; 12: 2241-2252.
Chen J, Hao Q, Zhang J et al. The efficacy and ocular safety following aflibercept, conbercept, ranibizumab, bevacizumab, and laser for retinopathy of prematurity: a systematic review and meta-analysis. Ital J Pediatr 2023; 49:136.
Stahl A, Nakanishi H, FIREFLEYE next Study Group et al. Intravitreal aflibercept vs laser therapy for retinopathy of prematurity: two-year efficacy and safety outcomes in the nonrandomized controlled trial FIREFLEYE next. JAMA Netw Open 2024; 7: e248383.
Downloads
Published
Issue
Section
License
Copyright (c) 2024 Consejo Argentino de Oftalmología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Con esta licencia no se permite un uso comercial de la obra original, ni la generación de obras derivadas. Las licencias Creative Commons permiten a los autores compartir y liberar sus obras en forma legal y segura.