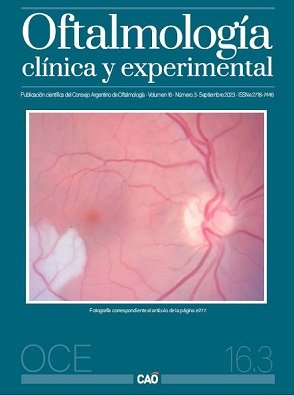
El microbioma y el ojo
¿es posible una oftalmología sistémica?
DOI:
https://doi.org/10.70313/2718.7446.v16.n03.239Palabras clave:
microbioma, ojo, oftalmología sistémica, inflamación, intestinoResumen
Los microorganismos del tracto intestinal pueden ser parte del origen o contribuir al desarrollo de ciertas enfermedades oculares, principalmente cuando se altera su equilibrio. Conocer estos aspectos implica comprender a la oftalmología más allá de los ojos. Algo que podrá tener implicancias tanto para el diagnóstico como para el desarrollo de nuevas estrategias terapéuticas. Esta revisión comparte conceptos que incentivan la relevancia de establecer abordajes multidisciplinarios en oftalmología.
Descargas
Referencias
Fasano A. All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases. F1000Research 2020; 9: F1000 Faculty Rev-69.
Farhadi A, Banan A, Fields J, Keshavarzian A. Intestinal barrier: an interface between health and disease. J Gastroenterol Hepatol 2003; 18: 479-497.
The Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature 2013; 486: 207-214.
Tringe SG, Rubin EM. Metagenomics: DNA sequencing of environmental samples. Nat Rev Genet 2005; 6: 805-814.
Fasano A. Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity and cancer. Physiol Rev 2011; 91: 151-175.
Dethlefsen L, McFall-Ngai M, Relman DA. An ecological and evolutionary perspective on human-microbe mutualism and disease. Nature 2007; 449: 811-818.
Moszak M, Szulinska M, Bogdansk P. You are what you eat: the relationship between diet, microbiota and metabolic disorders: a review. Nutrients 2020; 12: 1096.
Zheng D, Liwinski T, Elinav E. Interaction between microbiota and immunity in health and disease. Cell Research 2020; 30: 492-506.
Foster JA, McVey KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosc 2013; 36: 305-312.
Turnbaugh PJ, Ley RE, Hamady M et al. The human microbiome project. Nature 2007; 449: 804-810.
Carrasco-Ramiro F, Peiró-Pastor R, Aguado B. Human genomics projects and precision medicine. Gene Ther 2017; 24: 551-561.
Mörbe UM, Jørgensen PB, Fenton TM et al. Human gut-associated lymphoid tissues (GALT): diversity, structure and function. Mucosal Immunol 2021; 14: 793-802.
Caio G, Volta U, Sapone A et al. Celiac disease: a comprehensive current review. BMC Med 2019; 17: 142.
Wang L, Wang FS, Gershwin ME. Human autoimmune diseases: a comprehensive update. J Intern Med 2015; 278: 369-395.
Main BS, Minter MR. Microbial immuno-communication in neurodegenerative diseases. Front Neurosci 2017; 11: 151.
Wekerle H. The gut-brain connection: triggering of brain autoimmune disease by commensal gut bacteria. Rheumatol 2016; 55 (supp. 2): ii68-ii75.
Benakis C, Brea D, Caballero S et al. Commensal microbiota affects ischemic stroke outcome by regulating intestinal γδ T cells. Nat Med 2016; 22: 516-523.
Bonnie Bassler habla sobre cómo se comunican las bacterias [en línea]. Feb. 2009. Disponible en YouTube: https://www.ted.com/talks/bonnie_bassler_how_bacteria_talk?language=es
Margulis L, Bermudes D. Symbiosis as a mechanism of evolution: status of cell symbiosis theory. Symbiosis 1985; 1: 101-124.
Guerrero R, Margulis L, Berlanga MI. Symbiogenesis: the holobiont as a unit of evolution. Int Microbiol 2013; 16: 133-143.
Fasano A, Shea-Donohue T. Mechanisms of disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal autoimmune diseases. Nat Clin Pract Gastroenterol Hepatol 2005; 2: 416-422.
Prescott SL. Early-life environmental determinants of allergic diseases and the wider pandemic of inflammatory noncommunicable diseases. J Allergy Clin Immunol 2013; 131: 23-30.
Furman D, Campisi J, Verdin E et al. Chronic inflammation in the etiology of disease across the life span. Nature Medicine 2019; 25: 1822-1832.
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005; 352: 1685-1695.
Koren O, Spor A, Felin J et al. Human oral, gut, and plaque microbiota in patients with atherosclerosis. Proc Natl Acad Sci USA 2011; 108 (Suppl 1): 4592-4598.
Karlsson FH, Fåk F, Nookaew I et al. Symptomatic atherosclerosis is associated with an altered gut metagenome. Nature Commun 2012; 3: 1245.
Coussens LM, Werb Z. Inflammation and cancer. Nature 2002; 420: 860-867.
Taniguchi K, Karin M. NF-κB, inflammation, immunity and cancer: coming of age. Nat Rev Immunol 2018; 18: 309-324.
Hotamisligil GS. Inflammation and metabolic disorders. Nature 2006; 444: 860-867.
Dregan A, Charlton J, Chowienczyk P, Gulliford MC. Chronic inflammatory disorders and risk of type 2 diabetes mellitus, coronary heart disease and stroke. Circulation 2014; 130: 837-844.
Chimenti MS, Triggianese P, Conigliaro P et al. The interplay between inflammation and metabolism in rheumatoid arthritis. Cell Death Dis 2015; 6: e1887.
Ku IA, Imboden JB, Hsue PY, Ganz P. Rheumatoid arthritis: model of systemic inflammation driving atherosclerosis. Circ J 2009; 73: 977-985.
Franceschi C, Garagnani P, Parini P et al. Inflammaging: a new immune- metabolic viewpoint for age-related diseases. Nat Rev Endocrinol 2018; 14: 576-590.
Cryan JF, O’Riordan KJ, Cowan CSM et al. The microbiota-gut-brain axis. Physiol Rev 2019; 99: 1877-2013.
Marsland BJ, Trompette A, Gollwitzer ES. The gut-lung axis in respiratory disease. Ann Am Thorac Soc 2015; 12 (Suppl 2): S150-156.
Trujillo-Vargas CM, Schaefer L, Alam J et al. The gut-eye-lacrimal gland-microbiome axis in Sjögren syndrome. Ocul Surf 2020; 18: 335-344.
Napolitano P, Filippelli M, Davinelli S et al. Influence of gut microbiota on eye diseases: an overview. Ann Med 2021; 53: 750-761.
Montgomery TL, Künstner A, Kennedy JJ et al. Interactions between host genetics and gut microbiota determine susceptibility to CNS autoimmunity. Proc Natl Acad Sci USA 2020; 117: 27516-27527.
Moon J, Yoon CH, Choi SH, Kim MK. Can gut microbiota affect dry eye syndrome? Int J Mol Sci 2020; 21: 8443.
Lin P. The role of the intestinal microbiome in ocular inflammatory disease. Curr Opin Ophthalmol 2018, 29: 261-266.
Kodati S, Sen HN. Uveitis and the gut microbiota. Best Pract Res Clin Rheumatol 2019; 33: 101500.
Rosenbaum JT, Asquith M. The microbiome and HLA-B27-associated acute anterior uveitis. Nat Rev Rheumatol 2018; 14: 704-713.
Esser N, Legrand-Poels S, Piette J et al. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res Clin Pract 2014; 105: 141-150.
Wen L, Duffy A. Factors influencing the gut microbiota, inflammation, and type 2 diabetes. J Nutr 2017; 147: 1468S-1475S.
Kauppinen A, Paterno JJ, Blasiak J et al. Inflammation and its role in age-related macular degeneration. Cell Mol Life Sci 2016; 73: 1765-1786.
Rinninella E, Mele MC, Merendino N et al. The role of diet, micronutrients and the gut microbiota in age-related macular degeneration: new perspectives from the gut-retina axis. Nutrients 2018; 10: 1677.
Elhusseiny AM, Fakhari H, Bishehsari F et al. A gut connection in mucous membrane pemphigoid: insights into the role of the microbiome. Ocul Surf 2019; 17: 615-616.
Tsirouki T, Dastiridou A, Symeonidis C et al. A focus on the epidemiology of uveitis. Ocul Immunol Inflamm 2018; 26: 2-16.
Costello ME, Ciccia F, Willner D et al. Intestinal dysbiosis in ankylosing spondylitis. Arthritis Rheumatol 2015; 67: 686-691.
Mielants H, De Vos M, Cuvelier C, Veys EM. The role of gut inflammation in the pathogenesis of spondyloarthropathies. Acta Clin Belg 1996; 51: 340-349.
Fasano A. Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity and cancer. Physiol Rev 2011; 91: 151-175.
Sturgeon C, Fasano A. Zonulin, a regulator of epithelial and endothelial barrier functions and its involvement in chronic inflammatory diseases. Tissue Barriers 2016; 4: e1251384.
Napolitano P, Filippelli M, Davinelli S et al. Influence of gut microbiota on eye diseases: an overview. Ann Med 2021; 53: 750-761.
de Paiva CS, Jones DB, Stern ME et al. Altered mucosal microbiome diversity and disease severity in Sjogren syndrome. Sci Rep 2016; 6: 23561.
Malesza IJ, Malesza M, Walkowiak J et al. High-fat, Western-style diet, systemic inflammation and gut microbiota: a narrative review. Cells 2021; 10: 3164.
Sanders ME, Merenstein DJ, Reid G et al. Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nat Rev Gastroenterol Hepatol 2019; 16: 605-616.
Hill C, Guarner F, Reid G et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol 2014; 11: 506-514.
Gibson GR, Hutkins R, Sanders ME et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol 2017; 14: 491-502.
Vergés C, Ribas González V. Are microbiota and probiotics ready for use in Ophthalmology? Cataract Refract Surg Today Glob (Eur Ed) 2021: 26-30. Disponible en: https://crstodayeurope.com/articles/may-2021/are-microbiota-and-probiotics-ready-for-use-in-ophthalmology/
Hamilton MJ, Weingarden AR, Sadowsky MJ, Khoruts A. Standardized frozen preparation for transplantation of fecal microbiota for recurrent Clostridium difficile infection. Am J Gastroenterol 2012; 107: 761-767.
Damman CJ, Miller SI, Surawicz CM, Zisman TL. The microbiome and inflammatory bowel disease: is there a therapeutic role for fecal microbiota transplantation? Am J Gastroenterol 2012; 107: 1452-1459.
Layús BI, Gomez MA, Cazorla SI, Rodriguez AV. Drops of Lactiplantibacillus plantarum CRL 759 culture supernatant attenuates eyes inflammation induced by lipopolysaccharide. Benef Microbes 2021; 12: 163-174.
Layús BI, Gerez CL, Rodriguez AV. Development of an ophthalmic formulation with a postbiotic of Lactiplantibacillus plantarum CRL 759. Benef Microbes 2022; 13: 417-425.
Layús BI. Efecto anti-inflamatorio de una formulación postbiótica en un modelo de inflamación ocular [en línea]. Seminario de la Asociación de Investigación en Visión y Oftalmología Argentina (AIVO) 29 de junio de 2023. Disponible en YouTube: https://www.youtube.com/watch?v=HTF4s1JIuPM&t=10s
Shah I. Tales of the Dervishes: teaching-stories of the Sufi masters over the past thousand years: selected from the Sufi classics, from oral tradition, from unpublished manuscripts and schools of Sufi teaching in many countries. London: Octagon Press, 1967; p. 25-26.
NCD Countdown 2030 collaborators. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet 2018; 392: 1072-1088.
Saeedi P, Ptersohn I et al, IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract 2019; 157: 107843.
McDade TW. Early environments and the ecology of infammation. Proc Natl Acad Sci USA 2012; 109 (suppl. 2): 17281-17288.
Morris D. The naked ape: a zoologist’s study of the human animal. New York: McGraw-Hill, 1967. Edición en español: El mono desnudo: un estudio del animal humano. Barcelona: Plaza y Janés, 1970.
Morris D. The human zoo. London: Jonathan Cape, 1969. Edición en español: El zoo humano. Barcelona: Plaza y Janés, 1970.
Publicado
Número
Sección
Licencia
Derechos de autor 2023 Consejo Argentino de Oftalmología

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.
Con esta licencia no se permite un uso comercial de la obra original, ni la generación de obras derivadas. Las licencias Creative Commons permiten a los autores compartir y liberar sus obras en forma legal y segura.