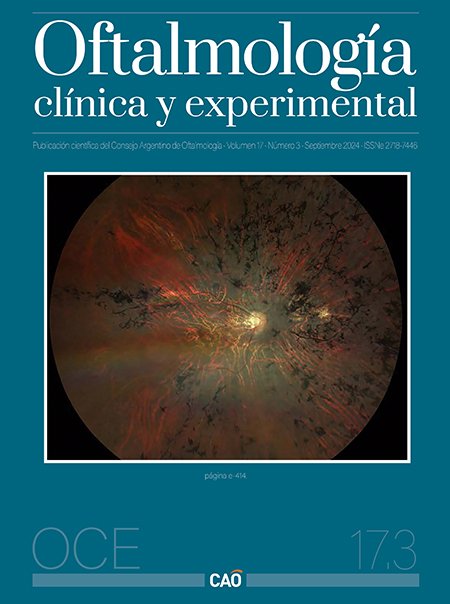
Visual, refractive and structural long-term results in premature infants treated for retinopathy of prematurity
DOI:
https://doi.org/10.70313/2718.7446.v17.n03.343Keywords:
retinopathy of prematurity, laser photocoagulation, antiangiogenic intravitreal injection, myopiaAbstract
Purpose: To analyze the best-corrected visual acuity, refractive state and anatomical long-term results in premature infants consecutively treated for ROP by laser photocoagulation and/or intravitreal injections of anti-angiogenic agents.
Methods: Retrospective analytical study. Those children treated for ROP since 1998 by laser photocoagulation, intravitreal injections of antiangiogenic agents, or both, and who had a minimum ophthalmological follow-up of three years post-treatment were included. Descriptive and frequency statistics were used, and the Chi-square test and Spearman’s correlation test were used for statistical association.
Results: 123 eyes of 62 patients were studied. The age at the last control was on average 9.66± 5.61 years. 116 eyes (94%) were treated by laser photocoagulation, 5 (4%) eyes required combined treatment, and 2 (2%) eyes with intravitreal injection of antiangiogenics. The mean spherical equivalent was -2.68±4.87 diopters, being significantly more negative in those with combined treatment (-11.54±2.36 D) and re-treatment (-12.46±3.26 D) and in those with posterior area disease (-7.50±5.49 vs +0.52±0.54 D) (p<0.01). Sixteen (15%) eyes were emmetropic, 32 (29%) eyes were hyperopic, and 62 (57%) eyes were myopic. 82 (74%) eyes had astigmatism and 20 (37%) patients had anisometropia. Sixty (60%) eyes had good visual acuity, 26 (25%) eyes had regular visual acuity and 16 (15%) had poor visual acuity. In 97 (80%) eyes the fundus did not present sequelae of the disease or other pathologies.
Conclusions: Most treated children retain good visual acuity, despite significant refractive errors, mainly myopia. The more posterior the disease, the higher the prevalence of high myopia.
References
Gupta A, Tripathy K. Central serous chorioretinopathy. En: StatPearls [en línea]. Treasure Island (FL): StatPearls Publishing, 2023 Aug. Disponible en: https://www.ncbi.nlm.nih.gov/books/NBK558973/
Fung AT, Yang Y, Kam AW. Central serous chorioretinopathy: a review. Clin Exp Ophthalmol 2023; 51: 243-270.
Park JB, Kim K, Kang MS et al. Central serous chorioretinopathy: treatment. Taiwan J Ophthalmol 2022; 12: 394-408.
Ivanišević M, Stanić R, Ivanišević P, Vuković A. Albrecht von Graefe (1828-1870) and his contributions to the development of ophthalmology. Int Ophthalmol 2020; 40: 1029-1033.
Rosen E. Central serous retinopathy. Am J Ophthalmol 1948; 31: 734.
Bennett G. Central serous retinopathy. Br J Ophthalmol 1955; 39: 605-618.
Kitzmann AS, Pulido JS, Diehl NN et al. The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980-2002. Ophthalmology 2008; 115: 169-173.
Facello Olmedo FM, Ormaechea G. Coriorretinopatía serosa central aguda y crónica: cambios coroideos observados con tomografía de coherencia óptica con imagen de profundidad mejorada. Oftalmol Clin Exp 2021; 14: 71-80.
Daruich A, Matet A, Dirani A et al. Central serous chorioretinopathy: recent findings and new physiopathology hypothesis. Prog Retin Eye Res 2015; 48: 82-118.
Daruich A, Matet A, Marchionno L et al. Acute central serous chorioretinopathy: factors influencing episode duration. Retina 2017; 37: 1905-1915.
Ficker L, Vafidis G, While A, Leaver P. Long-term follow-up of a prospective trial of argon laser photocoagulation in the treatment of central serous retinopathy. Br JOphthalmol 1988; 72: 829-834.
Gerendas BS, Kroisamer JS, Buehl W et al. Correlation between morphological characteristics in spectral-domain-optical coherence tomography, different functional tests and a patient's subjective handicap in acute central serous chorioretinopathy. Acta Ophthalmol 2018; 96: e776-e782.
Wang M, Munch IC, Hasler PW et al. Central serous chorioretinopathy. Acta
Ophthalmol 2008; 86: 126-145.
Yannuzzi NA, Mrejen S, Capuano V et al. A central hyporeflective subretinal lucency correlates with a region of focal leakage on fluorescein angiography in eyes with central serous chorioretinopathy. Ophthalmic Surg Lasers Imaging Retina 2015; 46: 832-836.
Iida T, Yannuzzi LA, Spaide RF et al. Cystoid macular degeneration in chronic central serous chorioretinopathy. Retina 2003; 23: 1-7, quiz 137-138.
Cardillo Piccolino F, Lupidi M, Cagini C et al. Choroidal vascular reactivity in central serous chorioretinopathy. Invest Ophthalmol Vis Sci 2018; 59: 3897-3905.
Sahoo NK, Mishra SB, Iovino C et al. Optical coherence tomography angiography findings in cystoid macular degeneration associated with central serous chorioretinopathy. Br J Ophthalmol 2019; 103: 1615-1618.
Mrejen S, Balaratnasingam C, Kaden TR et al. Long-term visual outcomes and causes of vision loss in chronic central serous chorioretinopathy. Ophthalmology 2019; 126: 576-588.
Spaide RF, Klancnik JM Jr. Fundus autofluorescence and central serous chorioretinopathy. Ophthalmology 2005; 112: 825-833.
Conrad R, Geiser F, Kleiman A et al. Temperament and character personality profile and illness-related stress in central serous chorioretinopathy. ScientificWorldJournal 2014; 2014: 631687.
Miki A, Kondo N, Yanagisawa S et al. Common variants in the complement factor H gene confer genetic susceptibility to central serous chorioretinopathy. Ophthalmology 2014; 121: 1067-1072.
Negi A, Marmor M.F. Experimental serous retinal detachment and focal pigment epithelial damage. Arch Ophthalmol 1984; 102: 445-449.
Nicholson B, Noble J, Forooghian F, Meyerle C. Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol 2013; 58: 103-126.
Spaide RF. Choroidal blood flow: review and potential explanation for the choroidal venous anatomy including the vortex vein system. Retina 2020; 40: 1851-1864.
Pang CE, Shah VP, Sarraf D, Freund KB. Ultra-widefield imaging with autofluorescence and indocyanine green angiography in central serous chorioretinopathy. Am J Ophthalmol 2014; 158: 362.e2-371.e2.
Brinks J, van Dijk EHC, Meijer OC et al. Choroidal arteriovenous anastomoses: a hypothesis for the pathogenesis of central serous chorioretinopathy and other pachychoroid disease spectrum abnormalities. Acta Ophthalmol 2022; 100: 946-959.
Imanaga N, Terao N, Nakamine S et al. Scleral thickness in central serous chorioretinopathy. Ophthalmol Retina 2021; 5: 285-291.
Fernández-Vigo JI, Moreno-Morillo FJ, Shi H et al. Assessment of the anterior scleral thickness in central serous chorioretinopathy patients by optical coherence tomography. Jpn J Ophthalmol 2021; 65: 769-776.
Sirakaya E, Duru Z, Kuçuk B, Duru N. Monocyte to high-density lipoprotein and neutrophil-to-lymphocyte ratios in patients with acute central serous chorioretinopathy. Indian J Ophthalmol 2020; 68: 854-858.
Zola M, Gobeaux C, Javorsky T et al. Galectin 3 and central serous chorioretinopathy: a promising new biomarker. Proc ARVO Annual Meeting 2021; 2021: 2197.
Bahadorani S, Maclean K, Wannamaker K et al. Treatment of central serous chorioretinopathy with topical NSAIDs. Clin Ophthalmol 2019; 13: 1543-1548.
Lehmann M, Bousquet E, Beydoun T, Behar-Cohen F. Pachychoroid: an inherited condition? Retina 2015; 35: 10-16.
Schubert C, Pryds A, Zeng S et al. Cadherin 5 is regulated by corticosteroids and associated with central serous chorioretinopathy. Hum Mutat 2014; 35: 859-867.
Zhang X, Lim CZF, Chhablani J, Wong YM. Central serous chorioretinopathy: updates in the pathogenesis, diagnosis and therapeutic strategies. Eye Vis (Lond) 2023; 10: 33.
Potsaid B, Baumann B, Huang D et al. Ultrahigh speed 1050 nm swept source/fourier domain OCT retinal and anterior segment imaging at 100,000 to 400,000 axial scans per second. Opt Express 2010; 18: 20029-20048.
Warrow DJ, Hoang QV, Freund KB. Pachychoroid pigment epitheliopathy. Retina 2013; 33: 1659-1672.
Gal-Or O, Dansingani KK, Sebrow D et al. Inner choroidal flow signal attenuation in pachychoroid disease: optical coherence tomography angiography. Retina 2018; 38: 1984-1992.
Burumcek E, Mudun A, Karacorlu S, Arslan MO. Laser photocoagulation for persistent central serous retinopathy: results of long-term follow-up. Ophthalmology 1997; 104: 616-622.
Roca JA, Wu L, Fromow-Guerra J et al. Yellow (577 nm) micropulse laser versus half-dose verteporfin photodynamic therapy in eyes with chronic central serous chorioretinopathy: results of the Pan-American Collaborative Retina Study (PACORES) Group. Br J Ophthalmol 2018; 102: 1696-1700.
Zeng M, Chen X, Song Y, Cai C. Subthreshold micropulse laser photocoagulation versus half-dose photodynamic therapy for acute central serous chorioretinopathy. BMC Ophthalmol 2022; 22: 110.
Yannuzzi LA, Slakter JS, Gross NE et al. Indocyanine green angiography-guided photodynamic therapy for treatment of chronic central serous chorioretinopathy: a pilot study. Retina 2003; 23: 288-298.
van Dijk EHC, Fauser S, Breukink MB et al. Half-dose photodynamic therapy versus high-density subthreshold micropulse laser treatment in patients with chronic central serous chorioretinopathy: the place trial. Ophthalmology 2018; 125: 1547-1555.
Manayath GJ, Narendran V, Arora S et al. Graded subthreshold transpupillary thermotherapy for chronic central serous chorioretinopathy. Ophthalmic Surg Lasers Imaging 2012; 43: 284-290.
Peiretti E, Caminiti G, Serra R et al. Anti-vascular endothelial growth factor therapy versus photodynamic therapy in the treatment of choroidal neovascularization secondary to central serous chorioretinopathy. Retina 2018; 38: 1526-1532.
Duan J, Zhang Y, Zhang M. Efficacy and safety of the mineralocorticoid receptor antagonist treatment for central serous chorioretinopathy: a systematic review and meta-analysis. Eye (Lond) 2021; 35: 1102-1110.
Daugirdas SP, Bheemidi AR, Singh RP. Should we stop treating patients with eplerenone for chronic CSCR?: commentary on the VICI trial. Ophthalmic Surg Lasers Imaging Retina 2021; 52: 308-310.
Feenstra HMA, van Dijk EHC, van Rijssen TJ et al. Long-term follow-up of chronic central serous chorioretinopathy patients after primary treatment of oral eplerenone or half-dose photodynamic therapy and crossover treatment: SPECTRA trial report No. 3. Graefes Arch Clin Exp Ophthalmol 2023; 261: 659-668.
Salehi M, Wenick AS, Law HA et al. Interventions for central serous chorioretinopathy: a network meta-analysis. Cochrane Database Syst Rev 2015; 2015: CD011841.
Gramajo AL, Marquez GE, Torres VE et al. Therapeutic benefit of melatonin in refractory central serous
horioretinopathy. Eye (Lond) 2015; 29: 1036-1045.
Lai TYY, Staurenghi G, Minerva Study Group et al. Efficacy and safety of ranibizumab for the treatment of choroidal neovascularization due to uncommon cause: twelve-month results of the Minerva Study. Retina 2018; 38: 1464-1477.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Consejo Argentino de Oftalmología

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Con esta licencia no se permite un uso comercial de la obra original, ni la generación de obras derivadas. Las licencias Creative Commons permiten a los autores compartir y liberar sus obras en forma legal y segura.