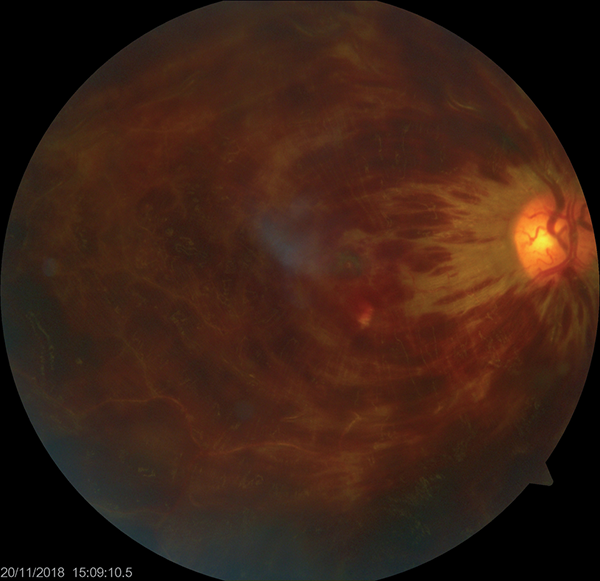
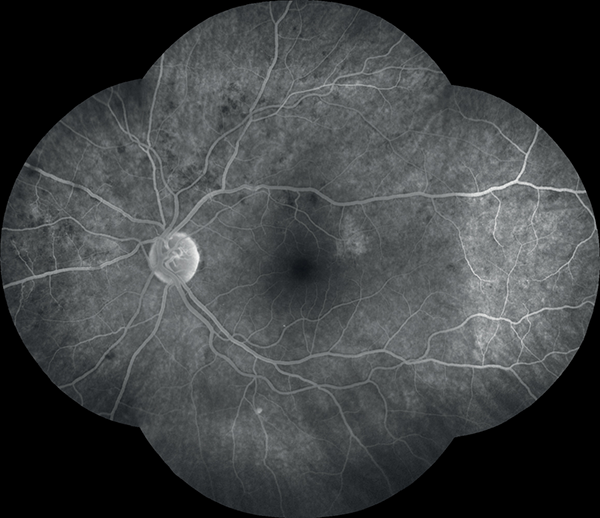
Figure 1. Retinography of the right eye shows central retinal vein occlusion.
Bilateral retinal vein occlusion in a patient with pulmonary arterial hypertension
María Lucía Urania, Matías Osabab, Fernando Antonio Vettorazzia
a Hospital Nacional de Clínicas, Facultad de Ciencias Médicas de la Universidad Nacional de Córdoba, Argentina.
b Facultad de Ciencias de la Salud, Universidad Católica de Córdoba, Argentina.
Received: March 15th, 2021.
Accepted: May 3rd, 2021.
María Lucía Urani, MD
marialuciaurani@gmail.com
Oftalmol Clin Exp (ISSN 1851-2658)
2021; 14(2): 109-115.
Statement of informed consent
Informed consent has not been obtained for this case report. However, the identity of the patient is not revealed.
Declaration of conflict of interest
The authors declare no potential conflicts of interest during the research about the authorship or the publication of this article.
Funding
The authors received no financial support for the research or publication of this article.
ABSTRACT
Purpose: to report a case of bilateral central retinal vein occlusion (CRVO) secondary to primary pulmonary arterial hypertension (PAH).
Case report: We performed a complete clinical and ophthalmological examination as well as fundoscopy, optical coherence tomography and fluorescein angiography. Pulmonary arterial hypertension was confirmed by catheterization of the pulmonary artery. Female patient had decreased visual acuity in both eyes in combination with respiratory insufficiency and peripheral cyanosis. The clinical condition and the results from the catheterization confirmed the diagnosis of bilateral CRVO secondary to PAH.
Conclusion: Bilateral CVRO can be one of the consequences of PAH and the treatment of the disease with vasodilators improves the prognosis and visual acuity.
Keyword: macitentan, ocular coherence tomography, central retinal vein occlusion, macular edema, primary pulmonary arterial hypertension.
Oclusión bilateral de vena retinal en paciente con hipertensión arterial pulmonar
RESUMEN
Objetivo: Describir una oclusión de vena central de la retina bilateral secundaria a hipertensión arterial pulmonar primaria.
Reporte del caso: Se realizó un examen clínico y oftalmológico completo a la paciente junto con fondo de ojo, tomografía de coherencia óptica y angiografía con fluoresceína. La cateterización de la arteria pulmonar confirmó el diagnóstico de la enfermedad de base. La paciente es una mujer de 27 años que se presentó a la guardia con disminución de la agudeza visual bilateral en combinación con disnea grado III y cianosis periférica. La cateterización, el examen clínico y oftalmológico confirmaron el diagnóstico de oclusión de la vena central de la retina bilateral secundaria a hipertensión arterial pulmonar primaria. El tratamiento instaurado para el edema macular fueron tres dosis de ranibizumab para el ojo derecho y el tratamiento para la enfermedad de base fue la utilización de macitentan 10 mg vía oral día.
Conclusión: La oclusión bilateral de vena central de la retina es una de las consecuencias oftalmológicas de esta enfermedad sistémica que el médico oftalmólogo debe de tener en cuenta. Además el tratamiento con macitentan intervendrá en la rápida recuperación de las consecuencias oftalmológicas al actuar sobre la patología de base de manera eficiente.
Palabras clave: macitentan, tomografía de coherencia óptica, oclusión de vena central de la retina, edema macular, hipertensión arterial pulmonar primaria.
Oclusão bilateral da veia retiniana em um paciente com hipertensão arterial pulmonar
RESUMO
Objetivo: Descrever uma oclusão bilateral da veia central retiniana secundária à hipertensão arterial pulmonar primária.
Reporte do caso: Realizou-se um exame clínico e oftalmológico completo na paciente, juntamente com fundo de olho, tomografia de coerência óptica e angiografia com fluoresceína. A cateterização da artéria pulmonar confirmou o diagnóstico da doença de base. A paciente é uma mulher de 27 anos que foi no serviço de urgências com diminuição da acuidade visual bilateral em combinação com dispneia grau III e cianose periférica. Cateterismo, exame clínico e oftalmológico confirmaram o diagnóstico de oclusão da veia central retiniana bilateral secundária à hipertensão arterial pulmonar primária. O tratamento estabelecido para o edema macular foi de três doses de ranibizumabe no olho direito e o tratamento para a doença de base foi o uso de macitentano 10 mg por via oral ao dia.
Conclusão: A oclusão da veia central retiniana bilateral é uma das consequências oftalmológicas desta doença sistêmica que o oftalmologista deve levar em consideração. Além disso, o tratamento com macitentan irá intervir na rápida recuperação das consequências oftalmológicas, agindo de forma eficiente na patologia subjacente.
Palavras chave: macitentan, tomografia de coerência óptica, oclusão da veia central da retina, edema macular, hipertensão arterial pulmonar primária.
INTRODUCTION
Pulmonary arterial hypertension (PAH) is a disease of the cardiopulmonary unit that affects the pulmonary arterial and venous circulation and the right ventricle of the heart. It produces an idiopathic obliteration of the pulmonary arterial capillaries which can cause an increase of the pulmonary vascular resistance and right ventricular afterload. These events promote right heart failure (RHF). Its incidence ranges from 2.0 to 7.5 cases per million per year and it has a higher female predilection. However, the major mortality rate is paradoxically higher in men than in women1-2.
The mean age at diagnosis is 37 years old with a median survival of 2.8 years if left untreated1. The diagnosis requires an assessment of pulmonary arterial pressure with a right heart catheterization1. Pulmonary hypertension is present when the mean pulmonary arterial pressure is greater than 25 mmHg at rest1. The main clinical aspects of the disease are: dyspnea, reduced exercise capacity, cyanosis, exertional syncope, and premature death from right heart failure. The treatment does not reduce the mortality; however, it reduces the hospitalization rate and increases the expectancy of life as well as the quality1. Vasodilators such as prostaglandins, phosphodiesterase inhibitors, endothelin receptors antagonist and soluble guanylate cyclase stimulators are used to control the symptoms1-2.
The development of PAH is secondary to dysregulation of vascular tone1. Due to Poiseuille’s law, changes in vessel radius translate into much greater vascular resistance1. These changes are mediated by vascular smooth muscle, which is influenced by three vasoactive molecules released by endothelial cells: nitric oxide (ON) and prostacyclin, which induce vasodilation, and endothelin which induce vasoconstriction. These mediators are in balance in order to preserve an optimal pulmonary vascular tone. The PAH is associated with reduced levels of prostacyclin and an increase in the vasoreactivity of ON and endothelin’s levels in plasma1-2. Agents that target the metabolism of ON via phosphodiesterase type 5 inhibition to increase cyclic guanosine monophosphate levels are an important target in the treatment of PAH. On the other hand, macitentan is a second generation endothelin receptor antagonist that acts selectively as a pulmonary vasodilator without the side effects noticed in the previous generation1. These groups of drugs are the main pathways to act in order to treat this affection3.
The RHF, which represents the last stage of the disease, produces an increase of vein pressure and venous stagnation which produces all the systemic complications of the PAH4. Rudolf Virchow described the factors contributing to thrombosis in the well-known Virchow’s triad, in which: venous stagnation, hypercoagulability and endothelial injury are the three broad categories that lead to thrombosis4.
These events, venous stagnation and the increase of vein blood pressure, produce choroidal and retinal venous congestion, which predisposes to retinal vein occlusion and other consequences such as retinal serous detachments and choroidal effusion. In addition to that, open angle glaucoma has also been described associated with serous detachments and vein occlusion in two different articles5-6. These last clinical aspects have been demonstrated in the published literature5-11.
Furthermore, one of the mechanisms in the pathogenesis of CRVO is the increase of the levels of the endothelin in the retinal environment. The increment is produced by stimulators like hypoxia and vein endothelial growth factor (VEGF). Kida et al. demonstrated the decrease of the levels of endothelin in plasma with a resolution of the macular edema and the improvement of visual acuity after the injection of bevacizumab12.
Taking this into account, the purpose of this work is to demonstrate bilateral CRVO as a consequence of the PAH in a young female patient and the treatment that was used to solve the complications of it.
CASE REPORT
A 27 years old woman entered the emergency room with bilateral several decreased vision within two days of evolution. She also had shortness of breath and signs of central and peripheral cyanosis. The patient denied any ocular and systemic condition at the interrogatory.
At the beginning, the best-corrected visual acuity was hand movement in the right eye and 20/400 in the left eye. The intraocular pressure, the cornea and the anterior chamber were normal. In the fundoscopy observation, there was a central vein occlusion with four quarters of intraretinal hemorrhage in the right eye. The fundus photograph in the left eye shows dilated and tortuous retinal veins in both superior and inferior quadrants with more intraretinal and nerve fiber layer hemorrhages in the superior pole, which also has cotton wool spots (Figs. 1 and 2).
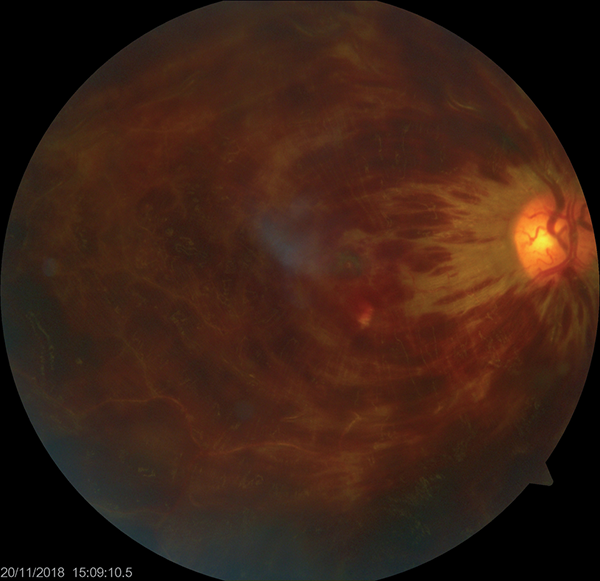
Figure 1. Retinography of the right eye shows central retinal vein occlusion.
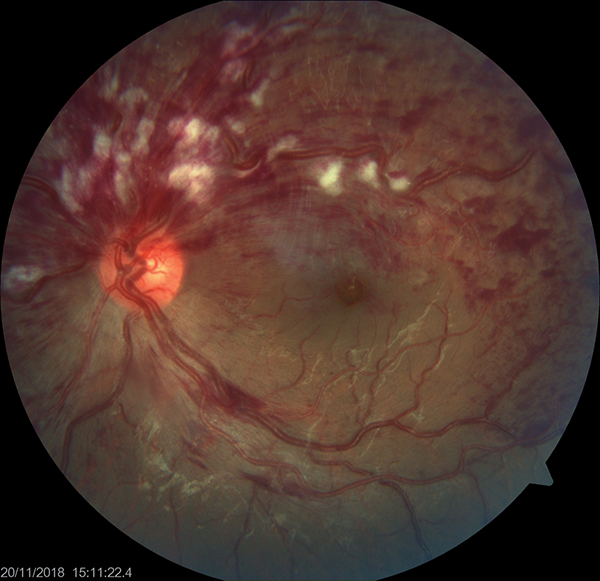
Figure 2. Retinography of the left eye shows a half central vein occlusion.
The patient was under hospitalization in the coronary unit for 10 days. The diagnosis of PAH with RHF was confirmed those days. The diagnosis was supported by the arterial catheterization. After being diagnosed, she was discharged from the hospital under medical treatment for that condition. The medical treatment was macitentan 10 mg per day.
The laboratory exams rejected other general diseases. The red blood cells, hematocrit and hemoglobin demonstrated a polyglobulia and the carbon dioxide and the oxygen pressures in the arterial blood confirmed respiratory insufficiency. An angiography was performed after two months of the episode showing a delay in the choroidal, arterial and venous circulation. There were no ischemic areas (Figs. 3 and 4). The OCT showed the macular alteration, principally in the right eye (Figs. 5 and 6).
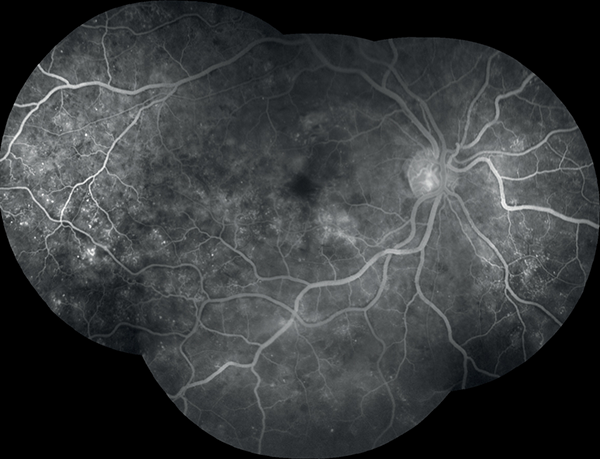
Figures 3 and 4. Fluorescein angiography of the right and left eyes without ischemic areas.
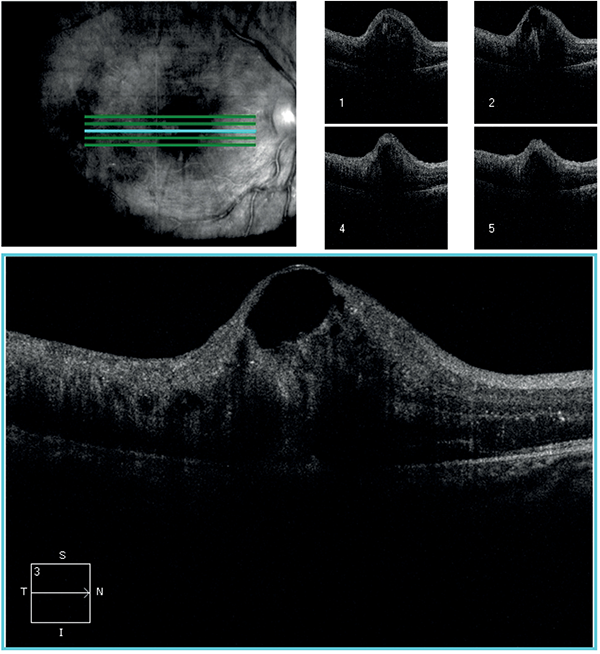
Figure 5. Spectral optical coherence tomography of the right eye showing increased macular thickening and macular edema. Central subfield is over 400 µm.
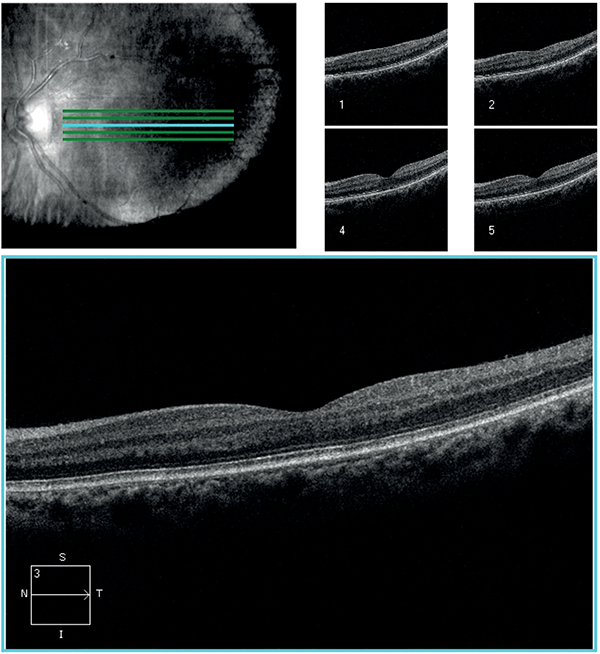
Figure 6. Spectral optical coherence tomography of the left with a central subfield thickness of 230 µm.
After four months of treatment the final visual acuity was 20/20 in both eyes with a central retina thickness (CRT) of 260 microns in both of them in the OCT after three months of treatment (Figs. 7 and 8). The dose of macitentan is 10 mg per day for life.

Figure 7. Spectral optical coherence tomography of the right after treatment.
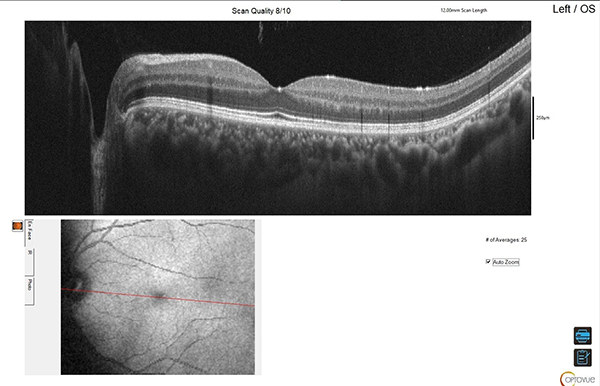
Figure 8. Spectral optical coherence tomography of the right and the left eye after treatment, final results.
DISCUSSION
The authors report a case of a female patient that presented a bilateral CRVO secondary PAH. The patient presented a decreased visual acuity in both eyes with symptoms of respiratory insufficiency. The diagnosis was confirmed by the arterial catheterization and the treatment with macitentan and three doses of ranibizumab in the right eye improved the visual outcomes of the patient as well as the systemic condition. The macular edema shown in the OCT improved with the use of three doses of ranibizumab with an improvement in the BVA to 20/20 and her systemic condition improved as well with the administration of the macitentan.
There have been reported in the literature some cases that demonstrated the clinical ophthalmological complications of PAH5-11. The complications of this pathology are choroidal effusion, serous retinal detachments, retinal vein occlusion, and open angle glaucoma. All of them are a consequence of right heart failure (RHF)5-11.
The RHF that appears in the last stages of the PAH produces a stagnation of blood flow and elevation of vein blood pressure. This outcome produces an increase in the ophthalmic superior vein pressure which leads to an increase in retinal venous pressure. The combination of high vein blood pressure with the stagnation of the blood flow are the main risk factors related to CRVO and, as we could see in this patient, both eyes can be affected in a short period of time.
As soon as the diagnosis was confirmed, the patient started the treatment with endothelin antagonist receptors, the macitentan. The treatment with macitentan can be one of the reasons for the improvement of visual acuity and the decrease of the CRT shown by OCT. This drug has a dual blockage action of endothelin receptors. This reduces vasoconstriction and hypertrophy of smooth muscle. In this way, it reduces retinal vein blood pressure and the venous stagnation which are the main risk factors that contribute to CRVO10.
On the other hand, Kida et al. showed in their work the increase of levels of endothelin in plasma and retinal tissue after CRVO9. Macitentan decreases those levels, lowering one of the factors that contribute in the pathogenesis of CRVO10. In this way, macitentan could be one of the causes of the improvement in the visual acuity and the resolution of the macular edema. Moreover, the use of ranibizumab in the right eye helped to gain the best visual outcomes.
Many articles have been published in the literature that demonstrated the outcomes of macitentan13-16. One of them is the article published by Belge et al. in 2019 in which macitentan had the best results in efficiency and safety compared with the others endothelin antagonist drugs (bosetentan, ambrisetan)14. Before this last one, Bedan et al. published an article that demonstrated that macitentan had fewer side effects than the other antagonist with a more secure profile15. On the other hand, Khan et al. published a case report about a patient with PAH treated with macitentan with cotton wools spots complications in the fundoscopic exam as a side effect of the drug16. This must be considered by the ophthalmologist as a complication of the drug.
Furthermore, the SHERAPIN study demonstrates that the patients treated with the combination therapy (macitentan + phosphodiesterase 5 inhibitors) reduce the mobility/mortality in 38% than the group with placebo and also reduces the hospitalization. However, the treatment in this patient was only with macitentan with an excellent systemic and ocular improvement11.
CONCLUSION
To summarize, the PHA has an important impact on visual health therefore; ophthalmologists have to be updated in the diagnosis and the treatment of it in order to preserve as much as possible the visual impairment. Macitentan is the goal standard drug to treat the PHA. Besides, it might have effects in the retinal environment. New research about macitentan related to ocular events could be studied in the future if this drug helps to improve the visual outcomes.
REFERENCES
1. Thenappan T, Ormiston ML, Ryan JJ, Archer SL. Pulmonary arterial hypertension: pathogenesis and clinical management. BMJ 2018; 360: j5492.
2. Thenappan T, Shah SJ, Rich S, Gomberd-Maitland M. A USA-based registry for pulmonary arterial hypertension. Eur Respir J 2007, 30: 1103-1110.
3. Monie DD, DeLoughery EP. Pathogenesis of thrombosis: cellular and pharmacogenetic contributions. Cardiovasc Diagn Ther 2017; 7 (suppl. 3): S291-S298.
4. Esmon CT. Basic mechanisms and pathogenesis of venous thrombosis. Blood Rev 2009; 23: 225-229.
5. Saran BR, Brucker AJ, Bandello F, Verougstraete C. Familiar primary pulmonary hypertension and associated ocular findings. Retina 2001; 21: 34-39.
6. Pham H, Akduman L, Kavali S. Bilateral central retinal vein occlusion in idiopathic pulmonary arterial hypertension. J Vitreoretin Dis 2018; 2: 183-187.
7. Beck R, Eckard A, Ewert R, Guthoff R. Netzhauterkrankungen bei primärer pulmonaler Hypertension [Retinal diseases with primary pulmonary hypertension]. Ophthalmologe 2003; 100: 732-735.
8. Nehemy MB, Torquetti L, Vasconcelos-Santos DV. Bilateral nonsimultaneous visual loss associated with idiopathic arterial pulmonary hypertension. Retin Cases Brief Rep 2010; 4: 154-157.
9. Senthil S, Kaur B, Jalali S, Garudadri C. Secondary open-angle glaucoma and central vein occlusion in a patient with primary pulmonary hypertension. Ophthalmic Surg Lasers Imaging 2009; 40: 50-53.
10. Saran BR, Brucker AJ, Bandello F, Verougstraete C. Familial primary pulmonary hypertension and associated ocular findings. Retina 2001; 21: 34-39.
11. Gupta I, Haddock L, Greenfield D. Secondary open-angle glaucoma and serous macular detachment associated with pulmonary hypertension. Am J Ophthalmol Case Rep 2020; 20: 100878.
12. Kida T. Mystery of retinal vein occlusion: vasoactivity of the vein and possible involvent of endothelin-1. Biomed Res Int 2017; 2017: 4816527.
13. Jansa P, Pulido T. Macitentan in pulmonary arterial hypertension: a focus on combination therapy in the SERAPHIN trial. Am J Cardiovasc Drugs 2018; 18: 1-11.
14. Belge C, Delcroix M. Treatment of pulmonary arterial hypertension with the dual endothelin receptor antagonist macitentan: clinical evidence and experience. Ther Adv Respir Dis 2019; 13: 1-13.
15. Bedan M, Grimm D, Wehland M et al. A focus on macitentan in the treatment of pulmonary arterial hypertension. Basic Clin Pharmacol Toxicol 2018; 123: 103-113.
16. Khan MA, Ho AC, Spirn MJ. Cotton-wool spots after use of macitentan for pulmonary arterial hypertension. Retin Cases Brief Rep 2017; 11: 4-6.