ORIGINAL ARTICLES
Short-term visual outcomes with the Magnificent intraocular lens: an Argentine exploratory study
Valentina María Rodríguez Martinia, Tomás Jaeschkeb, Fernando Mayorga Argañaraza-b
a Servicio de Oftalmología, Hospital Alemán, Buenos Aires, Argentina.
b Instituto de la Visión, Buenos Aires, Argentina.
Received: June 24th, 2025.
Approved: August 27th, 2025.
Corresponsal author
Dr. Fernando Mayorga Argañaraz
Servicio de Oftalmología
Hospital Alemán,
Av. Pueyrredón 1716
(C1119AAT) Ciudad de Buenos Aires
Argentina
+54 (11) 4490-0482
fernandommayorga@gmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2025; 18(3): e314-e320.
DOI: https://doi.org/10.70313/2718.7446.v18.n3.445
Conflict of interest
The authors declare no conflicts of interest.
Abstract
Objective: To explore the short-term visual outcomes following implantation of the Magnificent intraocular lens in patients undergoing cataract surgery in an Argentine cohort, evaluating its performance as an extended depth of focus (EDOF) lens.
Methods: This retrospective study analyzed clinical data from patients implanted with the Magnificent IOL. Uncorrected visual acuity (distance, intermediate, and near) at 30 days postoperatively and the spherical equivalent (SE) preoperatively and at 30 days were evaluated in right eyes, left eyes, and binocular vision. Intra- and intergroup comparisons were performed using paired t-tests and ANOVA.
Results: Data from 14 patients (28 eyes) were analyzed. A significant improvement in uncorrected visual acuity was observed at 30 days postoperatively across all distances. The mean binocular uncorrected visual acuity at distance was 0.01 LogMAR; for intermediate vision, 0.10; and for near vision, 0.18. The postoperative SE was within ±0.50 D in 93% of the eyes. Comparisons with preoperative values showed statistically significant differences (p<0.001). The lens demonstrated an optical performance pattern consistent with EDOF lens design.
Conclusion: The Magnificent IOL provided functional vision at all distances and good refractive predictability in this initial series. Prospective studies with longer follow-up are needed to confirm these findings and to definitively classify this lens as EDOF.
Keywords: intraocular lens, EDOF, Magnificent IOL, visual acuity, cataract surgery.
Resultados visuales a corto plazo con la lente intraocular Magnificent: un estudio exploratorio en población argentina
Resumen
Objetivo: Explorar los resultados visuales a corto plazo tras la implantación de la lente intraocular Magnificent en pacientes sometidos a cirugía de cataratas en una cohorte argentina, evaluando su desempeño como lente de profundidad de foco extendida (EDOF).
Métodos: Estudio retrospectivo basado en datos clínicos de pacientes operados con la lente Magnificent. Se analizaron la agudeza visual sin corrección a 30 días postoperatorios (lejos, intermedia y cercana) y el equivalente esférico preoperatorio y a los 30 días, en ojos derechos, izquierdos y binocular. Se realizaron comparaciones intra e intergrupales mediante pruebas t pareadas y ANOVA.
Resultados: Se evaluaron los datos de 14 pacientes (28 ojos) donde se observó una mejora significativa en la agudeza visual sin corrección a los 30 días en todas las distancias. En visión lejana binocular, el promedio fue 0,01 LogMAR; para visión intermedia, 0,10; y para visión cercana, 0,18. El equivalente esférico postoperatorio fue ≤ ±0,50 D en el 93% de los ojos. Las comparaciones con el preoperatorio mostraron diferencias estadísticamente significativas (p<0,001). La lente evidenció un patrón de desempeño óptico consistente con un diseño EDOF.
Conclusión: La lente Magnificent mostró resultados visuales funcionales a todas las distancias y buena predicción refractiva en esta serie inicial. Son necesarios estudios prospectivos con mayor seguimiento para confirmar estos hallazgos y su clasificación definitiva como lente EDOF.
Palabras clave: lente intraocular, EDOF, Magnificent, agudeza visual, cirugía de cataratas.
Resultados visuais de curto prazo com a lente intraocular Magnificent: um estudo exploratório em população argentina
Resumo
Objetivo: Explorar os resultados visuais de curto prazo após o implante da lente intraocular Magnificent em pacientes submetidos à cirurgia de catarata em uma coorte argentina, avaliando seu desempenho como uma lente de profundidade de foco estendida (EDOF).
Métodos: Estudo retrospectivo baseado em dados clínicos de pacientes operados com a lente Magnificent. A acuidade visual não corrigida (para longe, intermediária e perto) e a acuidade visual equivalente esférica pré-operatória e de 30 dias foram analisadas nos olhos direito, esquerdo e binocular. Comparações intra e intergrupos foram realizadas por meio de testes t pareados e ANOVA.
Resultados: Dados de 14 pacientes (28 olhos) foram avaliados, mostrando uma melhora significativa na acuidade visual não corrigida em 30 dias em todas as distâncias. Para a visão binocular à distância, a média foi de 0,01 LogMAR; para a visão intermediária, 0,10; e para a visão de perto, 0,18. O equivalente esférico pós-operatório foi ≤ ± 0,50 D em 93% dos olhos. As comparações com os dados pré-operatórios mostraram diferenças estatisticamente significativas (p < 0,001). A lente demonstrou um padrão de desempenho óptico consistente com um design EDOF.
Conclusão: A lente Magnificent apresentou resultados visuais funcionais em todas as distâncias e boa predição refrativa nesta série inicial. Estudos prospectivos com acompanhamento mais longo são necessários para confirmar esses achados e classificá-la definitivamente como uma lente EDOF.
Palavras-chave: lente intraocular, EDOF, Magnificent, acuidade visual, cirurgia de catarata.
Introduction
Over the past few decades, the development of intraocular lenses (IOLs) has evolved significantly, incorporating advanced optical designs that enhance postoperative visual quality beyond distance vision. Extended depth of focus (EDOF) lenses have emerged as an effective alternative to traditional multifocal lenses, as they provide a continuous range of vision from far to intermediate distances with a lower incidence of dysphotopic phenomena such as halos and glare1-3. In this context, technological innovation has led to the introduction of new models with modified aspheric profiles, hybrid diffractive elements, and even non-linear refractive solutions, aiming to maximize patient satisfaction during daily visual tasks such as using electronic devices or reading at functional distances4.
The Magnificent UHD intraocular lens (CareGroup, India) was first commercially introduced in Argentina in April 2022. Based on its optical behavior, it appears to belong to the EDOF segment, utilizing a hyper-aspheric design intended to extend the focal range without generating multiple images5-6. Its synchronized molding technology, combined with a hydrophobic acrylic material and blue light filter, was engineered to improve both optical performance and capsular stability. However, to date, no indexed scientific publications or independent clinical reports have been found evaluating its visual efficacy, highlighting the need for objective exploratory studies.
Given the increasing interest in visual solutions that preserve contrast sensitivity and minimize adverse effects, and the wide range of options available to ophthalmologists when choosing between monofocal plus and EDOF lenses, there is a clear need to conduct a short-term exploratory evaluation of the Magnificent lens in Argentine cataract patients, with the aim of describing its initial visual performance.
Methods
A retrospective study was conducted to analyze visual outcomes in cataract patients who received the Magnificent intraocular lens implant. The study adhered to the principles of the declaration of Helsinki. All patients provided written informed consent, authorizing the use of their anonymized clinical data for scientific and academic purposes.
Two experienced cataract surgeons, each with over 15 years of surgical practice, were invited to participate. They were asked to review medical records of patients in whom they had implanted the Magnificent lens, in order to analyze the clinical data described below. The study population included healthy patients with age-related cataracts who underwent cataract surgery with this specific lens model. Eyes with traumatic cataracts, active uveitis, need for combined glaucoma procedures, hypermature cataracts, a history of any type of corneal transplant, irregular corneas, or media opacities were excluded. Additionally, eyes with any history of retinal surgery or previous corneal refractive surgery were not included.
All surgeries were performed by the same two surgeons (FM and TJ), using phacoemulsification through a 2.4 mm corneal incision, followed by lens implantation. The procedures took place in two private ophthalmology centers in Buenos Aires, Argentina, between July 2024 and March 2025. IOL power calculations were targeted for postoperative emmetropia in all cases. Postoperative treatment consisted of a fixed combination of topical antibiotic and corticosteroid, administered for two weeks. Patients were evaluated on the first postoperative day, at 7 days, and at 30 days, after which they were formally discharged.
The spherical equivalent was recorded both preoperatively and one month after surgery. Uncorrected distance visual acuity (UDVA) and best-corrected distance visual acuity (CDVA) were assessed at each visit, along with uncorrected intermediate (66 cm) and uncorrected near (40 cm) visual acuity. All visual assessments were performed under standardized lighting conditions, with accurate measurement and control of viewing distances. Distance visual acuity was initially recorded using a decimal scale and later converted to a logarithmic scale (LogMAR) to allow direct comparison with intermediate and near vision values, which were obtained using logarithmic reading charts.
For data analysis, a descriptive and comparative statistical evaluation was performed using a structured spreadsheet database, later processed with XLMiner Analysis ToolPak (Frontline Systems Inc., Incline Village, NV, USA). Continuous variables, such as visual acuity and spherical equivalent, were expressed as mean, standard deviation (SD), and range. The analysis included preoperative and 30-day postoperative decimal visual acuity values. Comparisons between pre- and postoperative values were performed using paired parametric hypothesis testing (paired t-test), after confirming data normality with the Shapiro-Wilk test. To compare outcomes between right eyes (OD), left eyes (OS), and binocular vision (OU) at 30 days, one-way analysis of variance (ANOVA) was used, followed by Tukey’s post hoc test. Statistical significance was defined as p < 0.05.
Results
Of the 14 patients included (28 eyes), 10 were women and 4 were men, with a mean age of 71.1 ± 7.3 years (range: 62-86 years). All surgeries were uneventful. Spherical equivalents decreased significantly postoperatively. Preoperative mean values were: OD: +1.7 ± 0.19 D (range: -0.75 to +3.75); OS: +1.5 ± 1.2 D (range: -1.00 to +4.00). At one month postoperatively: OD: +0.17 ± 0.26 D (range: -0.25 to +0.50). OS: +0.08 ± 0.23 D (range: -0.25 to +0.25). Table 1 presents segmented visual acuity data for the OD, OS, and OU, across the different evaluation timepoints.
Table 1. Visual acuity outcomes at distance, intermediate, and near with the Magnificent IOL (all values are mean ± SD with range in parentheses).
Distance vision (LogMAR) |
Preop |
Day 1 |
Day 30 |
p-value |
OD |
0.4 ± 0.06 (0.9-0.1) |
0.1 ± 0.01 (0-0.18) |
0 ± 0.04 (0-0.18) |
<0.01 |
OS |
0.3 ± 0.09 (0.8-0.9) |
0.1 ± 0.01 (0-0.18) |
0 ± 0.08 (0-0.1) |
<0.01 |
OU |
0.3 ± 0.29 (0.8-0.9) |
0 ± 0.01 (0-0.1) |
0 ± 0.07 (0-0.1) |
<0.01 |
|
||||
Intermediate vision (LogMAR) |
Preop |
Day 1 |
Day 30 |
p-value |
OD |
0.7 ± 0.04 (0.4-1) |
0.18 ± 0.02 (0-0.4) |
0.1 ± 0.01 (0-0.2) |
<0.01 |
OS |
0.5 ± 0.09 (0.8-0.9) |
0.18 ± 0.01 (0-0.4) |
0.1 ± 0.01 (0-0.3) |
<0.01 |
OU |
0.3 ± 0.20 (0.1-0.8) |
0.18 ± 0.17 (0.4-0.9) |
0.1 ± 0.01 (0-0.3) |
<0.01 |
|
|
|
|
|
Near vision (LogMAR) |
Preop |
Day 1 |
Day 30 |
p-value |
OD |
1.0 ± 0.07 (0.8-1) |
0.3 ± 0.02 (0.1-0.5) |
0.2 ± 0.02 (0.1-0.4) |
<0.01 |
OS |
0.7 ± 0.02 (0.8-1) |
0.3 ± 0.02 (0.2-0.4) |
0.2 ± 0.03 (0.1-0.4) |
<0.01 |
OU |
0.7 ± 0.02 (0.7-1) |
0.3 ± 0.03 (0.18-0.5) |
0.18 ± 0.22 (0.1-0.4) |
<0.01 |
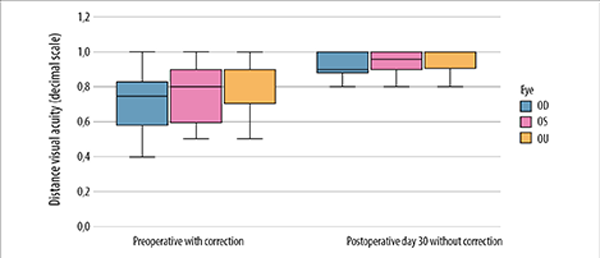
Figure 1 compares preoperative CDVA to postoperative UDVA at 30 days, using average decimal values. No eyes lost lines of vision. When comparing visual acuity outcomes among OD, OS, and OU at 30 days, no statistically significant differences were found (p=0.209). Figure 2 illustrates uncorrected visual acuity at 30 days postoperatively for distance, intermediate, and near vision, both monocular and binocular. A sustained improvement was observed across all distances, particularly under binocular conditions.
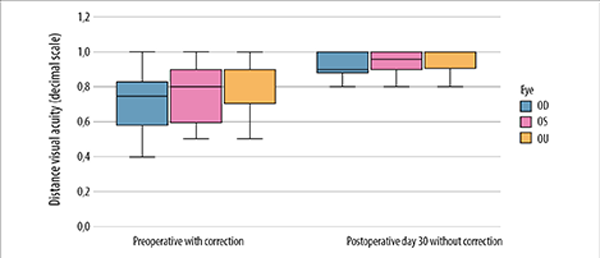
Figure 1. Distance visual acuity values before and one month after cataract surgery in patients implanted with the Magnificent intraocular lens. (OD: right eye. OS: left eye. OU: both eyes).
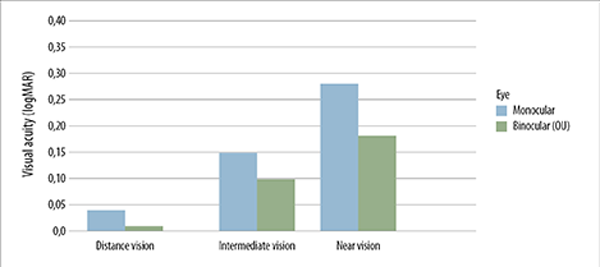
Figure 2. Uncorrected monocular and binocular visual acuity one month after surgery. Mean logMAR visual acuity values for distance, intermediate (66 cm), and near (33 cm) vision are presented in patients implanted with the Magnificent intraocular lens.
Discussion
The results of this exploratory study indicate that the Magnificent intraocular lens provides excellent uncorrected visual acuity at 30 days postoperatively for both distance and intermediate vision, along with acceptable near vision. Under binocular conditions, this translates into a high degree of spectacle independence for most patients. Although no statistically significant differences were observed between right eyes, left eyes, and binocular vision, the higher mean values in the OU group reflect an additional benefit from binocular summation, as previously reported with other EDOF designs. Considering that this study aimed for emmetropia in both eyes, it may be speculated that a mini-monovision strategy —leaving the non-dominant eye slightly myopic— could further enhance near performance, as suggested by Levy in a recent publication7.
Unlike diffractive or segmented-zone lenses, Magnificent is designed as a refractive lens with a progressive transition optic intended to provide extended depth of focus without inducing significant side effects such as halos or glare. This feature may be especially valuable in patients with high sensitivity to dysphotopsia or with demanding visual needs at multiple distances, as commonly encountered in modern daily activities (e.g., screen use, intermediate reading, driving). However, this study did not assess the presence or intensity of such clinical phenomena, and we are therefore unable to draw conclusions in this regard. We hope the present report will encourage future studies evaluating postoperative dysphotopsia over longer follow-up periods.
The 30-day follow-up period in this study corresponds to the typical clinical discharge timeline in routine practice. These were patients without complications, who are generally discharged after one month and usually return for annual follow-up. This opens the possibility for a future study assessing one-year outcomes, which would include evaluation of the long-term stability of the results reported here.
The lack of previously published peer-reviewed clinical studies on the Magnificent lens motivated us to analyze and share our preliminary findings in an Argentine patient population. From a methodological standpoint, this study was conducted under real-world clinical conditions, using accessible diagnostic tools such as decimal-scale visual acuity charts. However, near visual acuity was assessed using a logarithmic reading chart, allowing for more precise measurements and more reproducible reporting of outcomes.
Regarding the demographic characteristics of the study population, the small sample size limits generalizability. Nonetheless, this series included eyes with a strong tendency toward emmetropia, as reflected in the preoperative spherical equivalent values. At 30 days postoperatively, the mean refractive outcome was +0.17 D in right eyes and +0.08 D in left eyes, aligning closely with the intended emmetropic target. The favorable performance at multiple distances observed in this cohort raises the possibility that near vision outcomes could be further improved using a mini-monovision approach, without compromising distance vision. This strategy has shown promise with other monofocal-plus and EDOF lenses8-11.
This study presents several limitations that should be considered when interpreting the results. First, it is an exploratory observational analysis with a small sample size and short-term follow-up (30 days), which precludes assessment of refractive stability, neural adaptation, and visual performance under mesopic or scotopic conditions. All of these are important aspects for fully understanding the functional behavior of an IOL in clinical practice. Furthermore, this study did not include evaluation of subjective visual quality, presence of dysphotopsias, contrast sensitivity, or glare, which are essential components in the comprehensive characterization of any intraocular lens and in determining whether it meets the criteria to be classified as an EDOF lens. Finally, the study lacks a control group implanted with monofocal or traditional multifocal lenses, limiting the ability to make direct comparisons.
Conclusion
The preliminary findings of this study suggest that the Magnificent intraocular lens provides solid uncorrected visual performance at distance and intermediate ranges, along with satisfactory near vision. Outcomes were consistent in both right and left eyes, with a slight additional benefit observed under binocular conditions.
Despite the absence of prior indexed publications and the short follow-up period, these initial results are encouraging and support the need for larger-scale, prospective, controlled studies.
References
1. Karam M, Alkhowaiter N, Alkhabbaz A, Aldubaikhi A, Alsaif A, Shareef E, Alazaz R, Alotaibi A, Koaik M, Jabbour S. Extended depth of focus versus trifocal for intraocular lens implantation: an updated systematic review and meta-analysis. Am J Ophthalmol 2023; 251: 52-70. doi: 10.1016/j.ajo.2023.01.024.
2. van den Berg AB, van den Berg RM, Rocha KM, Chamon W, Waring GO 4th. Reading performance following contralateral implantation of an extended depth of focus (EDOF) IOL and a hybrid EDOF multifocal IOL. J Refract Surg 2024; 40(11): e778-e782. doi: 10.3928/1081597X-20240909-01.
3. Tavassoli S, Ziaei H, Yadegarfar ME, Gokul A, Kernohan A, Evans JR, Ziaei M. Trifocal versus extended depth of focus (EDOF) intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2024; 7(7): CD014891. doi: 10.1002/14651858.CD014891.pub2.
4. Packer M, Monteiro T, Schweitzer C, Rosen P. Prospective, randomized, controlled multicenter study of a monofocal extended depth of focus IOL compared to a standard aspheric monofocal IOL. J Cataract Refract Surg 2025 Apr 15. doi: 10.1097/j.jcrs.0000000000001672.
5. Care Group Magnificen information (Gujarat, India). Disponible en: https://caregroupiol.com/product/magnificent/
6. Información de Magnificent UHD Gamma Vision. Disponible en: https://gammavision.com.ar/lentes-intraoculares/rango-extendido/magnificent
7. Levy I, Shah RP, Mukhija R, Nanavaty MA. Outcomes of mini-monovision with monofocal, enhanced monofocal and extended depth-of-focus intraocular lenses. Front Med (Lausanne) 2025; 12: 1522383. doi: 10.3389/fmed.2025.1522383.
8. Beltraminelli T, Rizzato A, Toniolo K, Galli A, Menghini M. Comparison of visual performances of enhanced monofocal versus standard monofocal IOLs in a mini-monovision approach. BMC Ophthalmol 2023; 23(1): 170. doi: 10.1186/s12886-023-02920-6.
9. Fujita Y, Nomura Y, Itami E, Oshika T. A comparative study of mini-monovision, crossed mini-monovision, and emmetropia with enhanced monofocal intraocular lenses. Sci Rep 2025; 15(1): 916. doi: 10.1038/s41598-024-80663-0.
10. Iselin K, Kaufmann C, Schmid MK, Thiel M, Sanak F, Golla K, Hedinger YM. Patient-reported outcome measures for assessing spectacle independence after implantation of monofocal or extended depth of focus (EDOF) intraocular lenses with various degrees of monovision. Klin Monbl Augenheilkd 2025; 242(4): 363-371. doi: 10.1055/a-2559-0878.
11. Scarfone HA, Rodríguez EC, Riera J, Rufiner M, Charles M. Visual performance after bilateral implantation of a new enhanced monofocal hydrophobic acrylic intraocular lens targeted for mini-monovision. Life (Basel) 2025; 15(1): 64. doi: 10.3390/life15010064.