ORIGINAL ARTICLES
Prevalence of dry eye disease among medical students at an Argentinian university
Valentina Páeza, Iara Milena Báeza, Popea Cruz Funes Lópeza, Matías Osabaa-b, Víctor Reviglioa-b
a Facultad Ciencias de la Salud, Universidad Católica de Córdoba, Córdoba, Argentina.
b Instituto de la Visión Cerro, Sanatorio Allende, Córdoba, Argentina.
Received: July 17th, 2025.
Approved: August 27th, 2025.
Corresponsal author
Dr. Matías Osaba
Instituto de la Visión Cerro-Sanatorio Allende
Av. Rafael Núñez 5019
(5000) Córdoba, Argentina.
doctorosaba@gmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2025; 18(3): e337-e343.
DOI: https://doi.org/10.70313/2718.7446.v18.n3.444
Abstract
Objective: Dry eye disease (DED) is a multifactorial disorder of the ocular surface characterized by a loss of tear film homeostasis. This study aimed to determine the prevalence and associated factors of DED among medical students at Universidad Católica de Córdoba, Argentina.
Methods: A descriptive, cross-sectional, and analytical study was conducted in May 2025 using a digital survey that included the validated Ocular Surface Disease Index (OSDI) questionnaire.
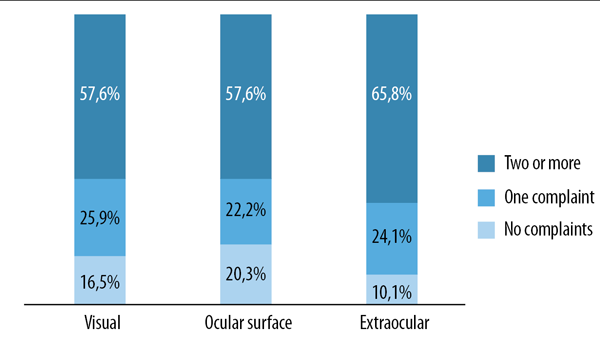
Results: A total of 158 responses were analyzed. Of these, 57.6% reported two or more visual symptoms, and 65.8% reported extraocular symptoms. Notably, 82% of respondents associated their symptoms with screen time. No significant associations were found with sex, academic year, or presence of refractive errors.
Conclusion: The findings highlight the high prevalence of symptomatic dry eye in young adults and underscore the need for preventive and educational measures promoting visual health in academic settings.
Keywords: digital screens, ocular symptoms, OSDI questionnaire, university students, visual display syndrome.
Prevalencia de la enfermedad del ojo seco entre los estudiantes de medicina de una universidad argentina
Resumen
Objetivo: La enfermedad del ojo seco (EOS) es un trastorno multifactorial de la superficie ocular que se caracteriza por una pérdida de la homeostasis de la película lacrimal. El objetivo de este estudio fue determinar la prevalencia y los factores asociados a la EOS entre los estudiantes de medicina de la Universidad Católica de Córdoba, Argentina.
Materiales y métodos: En mayo de 2025 se llevó a cabo un estudio descriptivo, transversal y analítico mediante una encuesta digital que incluía el cuestionario validado Índice de Enfermedad de la Superficie Ocular (OSDI).
Resultados: Se analizó un total de 158 respuestas. De ellas, el 57,6 % informó de dos o más síntomas visuales y el 65,8 % informó de síntomas extraoculares. Cabe destacar que el 82% de los encuestados asoció sus síntomas con el tiempo de exposición a pantallas. No se encontraron asociaciones significativas con el sexo, el año académico o la presencia de errores de refracción.
Conclusión: Los resultados ponen de relieve la alta prevalencia del ojo seco sintomático en adultos jóvenes y subrayan la necesidad de medidas preventivas y educativas que promuevan la salud visual en entornos académicos.
Palabras clave: pantallas digitales, síntomas oculares, cuestionario OSDI, estudiantes universitarios, síndrome visual informático.
Prevalência de olho seco entre estudantes de medicina de uma universidade argentina
Resumo
Objetivo: A doença do olho seco (DED) é uma doença multifatorial da superfície ocular caracterizada pela perda da homeostase do filme lacrimal. O objetivo deste estudo foi determinar a prevalência e os fatores associados à DED entre estudantes de medicina da Universidade Católica de Córdoba, Argentina.
Materiais e métodos: Foi realizado um estudo descritivo, transversal e analítico em maio de 2025, utilizando um questionário digital que incluiu o questionário validado Ocular Surface Disease Index (OSDI).
Resultados: Foram analisadas 158 respostas. Destas, 57,6% relataram dois ou mais sintomas visuais e 65,8% relataram sintomas extraoculares. Notavelmente, 82% dos entrevistados associaram seus sintomas ao tempo de tela. Não foram encontradas associações significativas com sexo, ano letivo ou presença de erros de refração.
Conclusão: Os resultados destacam a alta prevalência de olho seco sintomático em adultos jovens e reforçam a necessidade de medidas preventivas e educacionais para promover a saúde ocular em ambientes acadêmicos.
Palavras-chave: telas digitais, sintomas oculares, questionário OSDI, estudantes universitários, síndrome da visão computacional.
Introduction
Dry eye disease (DED) is a multifactorial disorder of the ocular surface characterized by tear film instability and loss of homeostasis1-2. Its symptoms include burning, irritation, blurry vision, foreign body sensation, photophobia, and itching3. The underlying pathophysiology may involve tear film hyperosmolarity, inflammation, epithelial damage, and, in some cases, neurosensory abnormalities4-5.
Historically, DED has been considered a condition predominantly affecting older individuals6-7. However, recent studies indicate a shift in the epidemiological profile, with increasing prevalence among young adults, particularly university students8-11. This trend may be attributed to prolonged screen exposure, academic stress, and environmental conditions that compromise tear film integrity12.
The rise in digital device use, especially in virtual education settings, has contributed to the emergence of computer vision syndrome (CVS), a condition marked by ocular discomfort and visual disturbances linked to extended screen time13. Medical students represent a high-risk group due to demanding study schedules and limited preventive measures14.
Prevalence rates of DED vary widely, ranging from 5% to 50%, depending on diagnostic criteria and contextual variables such as climate, lifestyle, and demographics15. In Latin America, particularly in Argentina, up to 50% of ophthalmologic consultations are related to complaints associated with DED16. International studies support this trend: in Serbia, DED symptoms were found in 60.5% of medical students, while in Poland, a 57.1% prevalence was reported, with correlations to screen time, allergies, and stress levels17.
Despite these findings, regional data remains limited. To our knowledge, no prior studies have investigated DED prevalence among medical students in Argentina. This study aims to fill that gap by determining the prevalence and associated factors of DED among medical students in Córdoba, Argentina.
Specific objectives include: assessing the frequency of DED symptoms using a validated survey (OSDI); comparing symptom prevalence among students with and without refractive errors; analyzing associations with screen time, gender, age, and academic year.
Materials and methods
This is a descriptive, cross-sectional, and analytical study. It included students from the School of Medicine at the Faculty of Health Sciences, Universidad Católica de Córdoba, from first-year to final-year (internship) students. The study was conducted during May 2025.
Participants were invited to complete an online survey distributed via WhatsAppTM using Google FormsTM. The survey gathered data on general health, digital screen use, and daily habits, and included the standardized Ocular Surface Disease Index (OSDI) questionnaire.
The OSDI is a validated patient-reported outcome measure (PROM) developed by Allergan Inc. to assess ocular surface disease. The current 12-item version evaluates the frequency and severity of ocular discomfort and visual limitations due to dry eye symptoms.
Responses are scored on a 0-4 scale (None to All the Time), with the option 'N/A' when not applicable. The total score is calculated by multiplying the sum of the responses by 25 and dividing by the number of valid responses, yielding a total score between 0 and 100.
Severity is classified as: Normal (0-12), Mild (13-22), Moderate (23-32), and Severe (33-100).
All students who agreed to participate were included after providing informed consent.
Ethical considerations
All participants provided informed consent at the start of the survey, which detailed the study’s purpose and ensured voluntary participation, anonymity, and confidentiality. The research protocol was approved by the Ethics Committee of Sanatorio Allende, Córdoba. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Statistical analysis
Descriptive statistical analysis was performed using tables, graphs, and summary measures. All analyses were conducted using R-medic software (http://www.r-medic.com/). A p-value of < 0.05 was considered statistically significant.
Results
A total of 158 medical students participated in the survey. The majority were female (79.1%). The most common age groups were 21-24 years (46.8%) and 18-20 years (41.1%). Participants were evenly distributed across different academic years, with a slight majority in the first year. Only 11.4% reported being smokers (Table 1).
Regarding sleep habits, 57% of students reported sleeping 7 hours per night, while 20.3% slept fewer than 6 hours.
Table 1. General characteristics of students interviewed (n=158).
According to the OSDI questionnaire, 57.6% of students reported two or more ocular symptoms, while 25.9% reported one symptom. Overall, 80% reported at least one ocular complaint (Fig. 1). Symptoms included blurry vision, visual fatigue, diplopia, difficulty refocusing, near vision discomfort, halos or glare, decreased clarity after screen use, and photophobia.
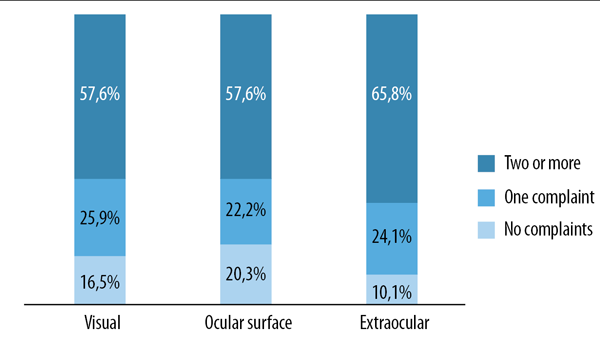
Figure 1. Distribution according to number and types of complaints (n=158).
As for extraocular symptoms, 65.8% reported two or more, and 24.1% reported one. The most common included headache, neck or shoulder pain, joint pain in hands or wrists, difficulty holding objects or writing, sleep disturbances, and attention problems.
When asked whether symptoms were related to screen time, 29% responded ‘always’, 53% ‘sometimes’, and 18% ‘rarely or never’. Regarding frequency, 43.7% described symptoms as ‘very frequent’, and 46.2% as ‘infrequent’.
Discussion
This study revealed a high prevalence of dry eye symptoms among medical students in Córdoba, Argentina, with 57.6% reporting multiple ocular complaints and 65.8% experiencing extraocular symptoms. These results align with international findings, where DED prevalence in similar populations ranges from 48% to 71%9-10,12, 18-19.
A key factor identified was excessive screen time13,20. In this sample, 82% of participants reported a link between symptoms and prolonged screen exposure21. This supports prior evidence indicating that more than four hours of daily screen use can destabilize the tear film through reduced blinking and increased evaporation22.
The post-pandemic academic environment has intensified digital device use20. The emergence of conditions like computer vision syndrome21 and ‘quarantine dry eye’22 reflects the multifactorial impact of screen exposure, indoor environments, and sedentary lifestyles23.
Although most respondents were female, no statistically significant gender differences were observed. While adult women are generally at higher risk due to hormonal influences, the young age of this sample may explain the lack of sex-based differences24.
There were also no significant associations between dry eye symptoms and academic year, refractive errors, or prior ocular conditions, suggesting that DED can occur independently of other visual disorders25.
The frequency of extraocular symptoms such as cervical pain, insomnia, and fatigue suggests a broader symptom complex related to digital overuse and poor ergonomics. This highlights the need for holistic interventions9.
The OSDI questionnaire effectively quantified symptom severity26 and provided current local data. The findings support preventive measures such as visual hygiene education, 20-20-20 breaks, ergonomic adjustments, and promotion of visual health in educational settings27.
Future studies should include clinical evaluations (Schirmer test, non-invasive tear breakup time, corneal staining), as well as variables like sleep quality, stress, and type of device used. Multicenter and prospective research could further clarify the epidemiology and public health impact of DED in students.
Conclusion
This study showed a high prevalence of symptoms compatible with dry eye disease (DED) in medical students, which highlights the importance of making this pathology visible in young populations. The application of the OSDI questionnaire allowed to identify that a significant proportion of students present symptoms, even in the absence of associated refractive pathology. The most relevant risk factors were prolonged use of screens, allergic history, use of contact lenses and sleep disturbances. Likewise, a positive relationship was observed between the time of exposure to electronic devices and the intensity of symptoms. Although no significant differences were found according to sex, age or year of study, these findings should be interpreted in the context of a predominantly young sample.
These results underscore the need to incorporate preventive strategies from the academic setting, such as education on visual hygiene, the promotion of active breaks (e.g., the 20-20-20 rule), and the promotion of healthy habits. Finally, it is recommended to move towards multicenter and prospective studies that integrate objective clinical evaluations, in order to understand more precisely the pathophysiology of dry eye syndrome in young people and its impact on quality of life and academic performance.
References
1. Wolffsohn JS, Travé-Huarte S, Stapleton F, Downie LE, Schulze MM, Guthrie S, Stahl U, Wang MTM, Craig JP. Relative importance of tear homeostatic signs for the diagnosis of dry eye disease. Ocul Surf 2025; 36: 151-155. doi: 10.1016/j.jtos.2025.01.010.
2. Wolffsohn JS, Benítez-Del-Castillo J, Loya-Garcia D, Inomata T, Iyar G, Liang L, Pult H, Sabater AL, Starr CE, Vehof J, Wang MT, Chen W, Craig JP, Dogru M, Quinones VLP, Stapleton F, Sullivan DA, Jones L; TFOS collaborator group. TFOS DEWS III Diagnostic Methodology. Am J Ophthalmol 2025 May 30:S0002-9394(25)00275-2. doi: 10.1016/j.ajo.2025.05.033.
3. Cheong N, Ang JH, Kaya C, Kumar A, Lam SSW, Tong L. Symptomology and impact of dry eye disease: a patient and physician perspective. Ophthalmol Ther 2025; 14(7): 1357-1368. doi: 10.1007/s40123-025-01166-3.
4. Li J, Bao X, Guo S, Huang Y, Huang C, Hu J, Liu Z. Cell death pathways in dry eye disease: insights into ocular surface inflammation. Ocul Surf 2024; 34: 535-544. doi: 10.1016/j.jtos.2024.11.004.
5. Bhujbal S, Rupenthal ID, Steven P, Agarwal P. Inflammation in dry eye disease-pathogenesis, preclinical animal models, and treatments. J Ocul Pharmacol Ther 2024; 40(10): 638-658. doi: 10.1089/jop.2024.0103.
6. Kitazawa K, Inomata T, Shih K, Hughes JB, Bozza N, Tomioka Y, Numa K, Yokoi N, Campisi J, Dana R, Sotozono C. Impact of aging on the pathophysiology of dry eye disease: a systematic review and meta-analysis. Ocul Surf 2022; 25: 108-118. doi: 10.1016/j.jtos.2022.06.004.
7. You L, Lin Y, Zheng Y, Han Z, Zeng L, Chen H. The impact of aging on ocular diseases: unveiling complex interactions. Aging Dis 2024; 16(5): 2803-2830. doi: 10.14336/AD.2024.0850.
8. Yang I, Wakamatsu T, Sacho IBI, Fazzi JH, de Aquino AC, Ayub G, Rebello PA, Gomes JÁP, Alves M. Prevalence and associated risk factors for dry eye disease among Brazilian undergraduate students. PLoS One 2021; 16(11): e0259399. doi: 10.1371/journal.pone.0259399.
9. Al-Zubi KM, Al-Kubaisy WA, Al-Azzeh YE, Batayneh BK, Alqaraleh HA, Abid LA, Al-Jadid Al-Majali GO, Alhajaj NT. Symptomatic dry eye disease among university students. Med Hypothesis Discov Innov Ophthalmol 2023; 12(2): 70-77.
10. Supiyaphun C, Jongkhajornpong P, Rattanasiri S, Lekhanont K. Prevalence and risk factors of dry eye disease among University Students in Bangkok, Thailand. PLoS One 2021; 16(10): e0258217. doi: 10.1371/journal.pone.0258217.
11. Tilahun MM, Alemayehu HB, Eticha BL, Mersha GA, Tegegn MT, Zeleke TC, Abdulkadir NH, Jara AG, Yalew ES, Tsegaye KB, Lorato MM. Symptomatic dry eye disease and associated factors among postgraduate students at Hawassa University, Sidama Region, Ethiopia. Sci Rep 2025; 15(1): 17356. doi: 10.1038/s41598-025-97928-x.
12. Lulla NH, Loganathan M, Balan VGM, Swathi S. Dry eye among medical students before and during COVID-19. Indian J Ophthalmol 2023; 71(4): 1468-1471. doi: 10.4103/IJO.IJO_2786_22.
13. Luo CK, Tan QQ, Tea Y, Pang Y. The prevalence of dry eye disease symptoms and its association with screen time in young adults aged 21-30 years. Ophthalmic Physiol Opt 2025; 45(5): 1195-1200. doi: 10.1111/opo.13505.
14. García-Ayuso D, Di Pierdomenico J, Moya-Rodríguez E, Valiente-Soriano FJ, Galindo-Romero C, Sobrado-Calvo P. Assessment of dry eye symptoms among university students during the COVID-19 pandemic. Clin Exp Optom 2022; 105(5): 507-513. doi: 10.1080/08164622.2021.1945411.
15. Britten-Jones AC, Wang MTM, Samuels I, Jennings C, Stapleton F, Craig JP. Epidemiology and Risk Factors of Dry Eye Disease: Considerations for clinical management. Medicina (Kaunas) 2024; 60(9): 1458. doi: 10.3390/medicina60091458.
16. Marini MC, Liviero B, Torres RM, Galperin G, Galletti JG, Alves M. Epidemiology of dry eye disease in Argentina. Discov Public Health 2024; 21: 59. https://doi.org/10.1186/s12982-024-00185-y.
17. Zeleke TC, Adimassu NF, Alemayehu AM, Dawud TW, Mersha GA. Symptomatic dry eye disease and associated factors among postgraduate students in Ethiopia. PLoS One 2022; 17(8): e0272808. doi: 10.1371/journal.pone.0272808.
18. Gupta P, Bansal A, Aggarwal A, Singla R. Study of face mask-associated dry eye among medical students. Int J Appl Basic Med Res 2023; 13(4): 240-245. doi: 10.4103/ijabmr.ijabmr_366_23.
19. Mamoon I, Ayub F, Sarwat S. Prevalence of dry eye disease among IT students in Pakistan. Int Ophthalmol 2024; 44(1): 204. doi: 10.1007/s10792-024-03142-5.
20. Aćimović L, Stanojlović S, Kalezić T, Dačić Krnjaja B. Evaluation of dry eye symptoms and risk factors among medical students in Serbia. PLoS One 2022; 17(10): e0275624. doi: 10.1371/journal.pone.0275624.
21. Cartes C, Segovia C, Salinas-Toro D, Goya C, Alonso MJ, Lopez-Solis R, Zapata C, Cabezas M, Yañez P, Flores-Rodriguez P, Lopez D, Matus G, Traipe L. Dry eye and visual display terminal-related symptoms among university students during the coronavirus disease pandemic. Ophthalmic Epidemiol 2022; 29(3): 245-251. doi: 10.1080/09286586.2021.1943457.
22. Saber Sahih Alnasab S, Asharlous A, Doostdar A, Nabovati P, Yekta A, Khabazkhoob M. Epidemiology of dry eye and its determinants among university students. J Ophthalmic Vis Res 2022; 17(3): 447-448. doi: 10.18502/jovr.v17i3.11586.
23. Wróbel-Dudzińska D, Osial N, Stępień PW, Gorecka A, Żarnowski T. Prevalence of dry eye symptoms and associated risk factors among university students in Poland. Int J Environ Res Public Health 2023; 20(2): 1313. doi: 10.3390/ijerph20021313.
24. Aberame AR, Bhandary SV, Rao LG, Gupta C. Assessment of prevalence of dry eye among medical students using ocular surface disease index questionnaire: is COVID-19 to be really blamed? Indian J Ophthalmol 2023; 71(4): 1450-1453. doi: 10.4103/IJO.IJO_2824_22.
25. Abdulmannan DM, Naser AY, Ibrahim OK, Mahmood AS, Alyoussef Alkrad J, Sweiss K, Alrawashdeh HM, Kautsar AP. Visual health and prevalence of dry eye syndrome among university students in Iraq and Jordan. BMC Ophthalmol 2022; 22(1): 265. doi: 10.1186/s12886-022-02485-w.
26. Uwimana A, Ma C, Ma X. Concurrent rising of dry eye and eye strain symptoms among university students during the COVID-19 pandemic era: a cross-sectional study. Risk Manag Healthc Policy 2022; 15: 2311-2322. doi: 10.2147/RMHP.S388331.
27. Basnet A, Thapa S, Ghising K, Shah SK, Pathak SB, Pradhan P. Assessment of symptomatic dry eye disease among postgraduate medical students of KIST Medical College and Teaching Hospital using an Ocular Surface Disease Index Questionnaire. Kathmandu Univ Med J (KUMJ) 2024; 22(85): 65-69.