ORIGINAL ARTICLE
Preliminary results of a IPCL phakic lens vault pilot study under different lighting conditions
Germán Roberto Bianchi MD, Daniel Ignacio del Campo MD, and Aura Bracho González MD
Clínica de Ojos Dr. Nano, Centro Panamericana, Blas Parera 4201, Olivos (Buenos Aires province), Argentina.
Received: December 11st, 2020.
Accepted: January 28th, 2021.
Corresponding author
Dr. Germán Roberto Bianchi
drbianchigerman@gmail.com
Oftalmol Clin Exp (ISSN 1851-2658)
2021; 14(1): e1- e13.
Acknowledgments
To María José Maldonado, for her great capability of team work, her unconditional and always good predisposition, as well as her constant administrative assistance for all these tasks, which facilitated the success observed in the patient satisfaction, in addition to the possibility of performing scientific studies as the present one.
ABSTRACT
Objective: To evaluate a posterior chamber phakic lens vault and its possible changes under different lighting conditions.
Materials and methods: A prospective case-series study was performed on 44 eyes (22 patients) operated with a phakic lens IPCL V2.0, between January and December of 2018, under three different lighting conditions (mesopic/scotopic/photopic). The central vault was measured with an optic coherence tomograph. The results obtained one and 2 years after surgery were compared, and the differences between the scotopic and the photopic condition was evaluated. Demographic aspects were also evaluated, as well as lens characteristics, endothelial cell density and central corneal thickness, as well as cataracts development.
Results: The mean age was 37 ± 9.7 years old; preoperative spherical equivalent: -8.4 ± 3.5 D; anterior chamber depth: 3.46 ± 0.28 mm; optic power: -8.9 ± 3.4 D. Endothelial cell density and central corneal thickness decreased 72.6 cells/mm² (p=0.15) and 0.5 mm (p=0.86), respectively. Two years after surgery, vault values were 582.6 ± 192.4 µm (mesopic); 635.3 ± 240.5 µm (scotopic) and 536.9 ± 216 µm (photopic), with no statistically significant changes when compared to results obtained one year after surgery (p=0.27, 0.72, 0.92, respectively). The vault difference observed between the scotopic and the photopic condition was 98.4 ± 48.4 µm, (p=0.001). Two years after surgery, no cataracts were detected.
Conclusions: The IPCL V2.0 phakic lens vault remained stable 2 years after surgery. Statistically significant differences were found when comparing the scotopic and the photopic lighting conditions. Cataracts, however, were not detected.
Key words: vault, phakic lens, complications, cataracts, photopic, scotopic, refractive surgery.
INTRODUCTION
Posterior chamber phakic lenses (located behind the iris and in front of the lens) are a safe and effective option for correcting refractive errors, especially when corneal procedures are counterindicated1-3. Moreover, they could have additional advantages, such as avoiding corneal wound healing and structural problems that can affect quality of sight4. However, the main concern of posterior chamber phakic lens is the possibility of cataract development. This is because, if they are too close to the lens, there could be contact between them, not only during the implantation procedure, but also in the years after surgery, due to the physiological movement of the accommodation process1-2, 5-7. Because of this, and in addition to preoperative measurements of the anterior chamber, postoperative measurements are also necessary in order to evaluate the distance between the posterior face of the phakic lens, and the anterior face of the crystalline lens, a parameter known as “vault”, which represents the real space remaining between the intraocular lens (IOL) and the crystalline lens.
Regarding the potential problem associated to corneal endothelial cells loss, and corneal dis-compensation, which occurred with different anterior chamber phakic lenses models8-10, seems to be a very unusual complication in the case of posterior chamber phakic lenses1-2, 10-11. The “Implantable Collamer Lens” (ICL), from the STAAR Surgical Company (Monrovia, CA) is the posterior chamber phakic lens that has been the longest on the market, with publications addressing its safety and effectivness1-3. There is also a more recent product called the “Implantable Posterior Contact Lens” (IPCL), from the Care Group (India), which other authors have evaluated12-13 as well as the author of this study, who obtained good visual results, without problems related to ocular pressure (the new lens design facilitates aqueous humor circulation), corneal endothelial or the crystalline lens14, even with a new variant with a diffractive optics for presbyopia correction15.
There are available studies which have analyzed vault changes under different lighting conditions and accommodation for ICLs lens16-20. However, we have not been able to find similar studies for the IPCL lens. Because of this, our purpose was to evaluate preliminary results regarding IPCL vault and its possible changes under different lighting conditions in myopic patients, 1 and 2 years after surgery.
METHODS
A prospective case-series, observational nonrandomized study was designed with 44 eyes from 22 patients (both eyes operated). Surgeries were performed between January and December of 2018, on patients who were implanted with IPCL V 2.0 phakic lenses with different models (toric, spherical, diffractive). The study protocol was evaluated and approved by the Institutional Review Board of the “Clínica de Ojos Dr. Nano”, and the work was developed following the principles established in the Declaration of Helsinki. An informed consent was obtained from all participants, who were informed that, in addition to standard postoperative evaluations, they would undergo “extra” studies under different lighting-controlled conditions, with the purpose of obtaining more scientific information of the implanted lens.
The eyes of myopic patients were selected in line with the inclusion/exclusion criteria previously published for implanting posterior phakic lens14, who agreed to participate in order to receive the postoperative measurements that we will now describe, at their first and second year follow-up appointment after surgery, if they have not developed any crystalline lens and/or corneal complications at their first annual evaluation. An optical coherence tomograph (OCT) equipment, with an anterior segment system (Topcon® DRI-OCT-1 Triton), was used to evaluate different anterior segment parameters. The main outcome was ICPL vault, evaluating the right eye first, and then the left eye, under three different lighting conditions, which were standardized with the aid of a luxmeter (Jieli® Lx-1010b), placing their sensor at 120 cm above the floor, in a vertical position (simulating the ocular globe position), trying to get the real altitude and position the head (and eyes) of the patient had at the time the OCT measurements were taken.
Controlled lighting conditions
Light condition A (mesopic), 400 LUX: this the intensity of light obtained when the lights of the patient room are turned on. It was standardized to represent normal working conditions in order to assess the OCT evaluation.
Light condition B (scotopic), 0.5 LUX: after performing the mesopic measurement, the lights of the patient room was turned off, obtaining a dim lit in a standardized condition. This light came only from the OCT screen while the measurement was performed.
Light condition C (photopic), 1500 LUX: finally, after turning the lights of the patient room on again, waiting 5 minutes with the head of the patient positioned to perform the OCT measurements, the counter-lateral eye (the one that it was not measured) was directly illuminated for 5 seconds from a distance of 15 cm with a white led flashlight (from a cell phone). Registering an intensity of 1500 LUX, pupil miosis was produced in the illuminated eye and, also in the other eye (which was under the OCT evaluation), due to the consensual reflex.
*Likewise, after registering the result in an electronic data-base, IPCL vault shifting was calculated (as the difference obtained between the value of the scotopic vault minus that of the photopic vault), at the one- and two-years marks after surgery.
Other evaluated parameters
In regards to the demographics of the populated that was studied, the following data was registered: age, gender, spherical equivalent (before surgery, and then one and two years after the procedure), anterior chamber depth, measured from the corneal endothelial to the anterior face of the crystalline lens, at its central point (evaluated by a Pentacam system; Oculus®, Wetzlar, Germany), the white-to-white distance (evaluated by a digital caliper, and also with an IOL-Master® 500 equipment; Carl Zeiss, Germany), which was necessary in order to select the adequate IPCL lens diameter and its optical power (information obtained using an online software provide by the ICPL manufacturer for registered surgeons). Endothelial cell density and central corneal thickness (before surgery, one and two years after the procedure) were also evaluated with an electronic specular microscope (TOMEY® EM4000). Finally, the presence of cataracts was evaluated in every annual control by slit lamp, according to the LOCS III classification system grade. Another evaluation, conducted at the baseline and the postoperative stage (one and two years after surgery) was the ultrabiomicroscopy (UBM) of the anterior segment (AvisoTM®; Quantel Medical), which is useful to measure the central and peripheral vault, obtaining information needed to rule out the possibility of any contact with the IPCL lens. All surgical procedures were performed by the same surgeon (GRB), as well as all postoperative evaluations, even if the OCT and the specular microscopy measurements were developed by other physicians from the present study group. The IPCL characteristics and the surgical technique were the same as has been previously published14.
A descriptive statistic evaluation was performed in order to process the information, presenting the results as “mean, standard deviation and range”. The Analysis of Varianza (ANOVA) simple factor test was used to calculate the difference between mean values of the endothelial cell density, and the central corneal thickness. The same test was used to see if there were any differences between the “vault values” obtained each year under mesopic, scotopic and photopic conditions. In order to evaluate vault stability through time, a paired “t test” was used to compare results obtained between the first and the second postoperative years, at different lighting conditions, and always considering results where p < 0,05 as evidence of a statistically significant difference.
RESULTS
From the total of 22 patients evaluated, 6 were men and the rest were women, with a mean age of 37 ± 9.7 years old (22-54). Regarding the anatomical characteristics of the eyes, anterior chamber depth was 3.46 ± 0.28 mm (2.92-3.85), with a white-to-white distance of 12.1 ± 0.3 mm (11.3-13), whereas the IPCL diameters of the used lenses was 12.9 ± 0.3 mm (12.2-13.7). In 12 patients (24 eyes), the IPCL implanted models were: V2.0 (12 eyes) and VT 2.0 (12 eyes) for correcting astigmatism. Meanwhile, the others 10 patients were implanted with diffractive models: 12 eyes only with spherical models, and 8 with the toric lens model (DT), for correcting astigmatism. The mean optical power of all implanted lenses was -8.9 ± 3.4 D (-3 a -17), wheras the mean cylinder for the toric models was 2.5 ± 0.9 D (1 to 4.5). For diffractive IPCL lenses, the mean value of the addition was 2.8 ± 0.9 D (1.5 a 4).
Table 1 shows the obtained improvement of the mean spherical equivalent, which is statistically significant. In the same chart, we can see the results of the endothelial cells density and the central corneal thickness, which remained stable, without statistically significant changes. The reduction of endothelial cell density was 72.6 cel/mm² (p=0.15), whereas the central corneal thickness registered a drop of 0,5 mm (p=0,86), two years after surgery. In addition, changes in the aspect of the crystalline lens from the evaluated cases (cataracts were not detected) were not detected, and the UBM evaluation did not show areas of contact between the crystalline lens and the IPCL lens (centrally or peripherally).
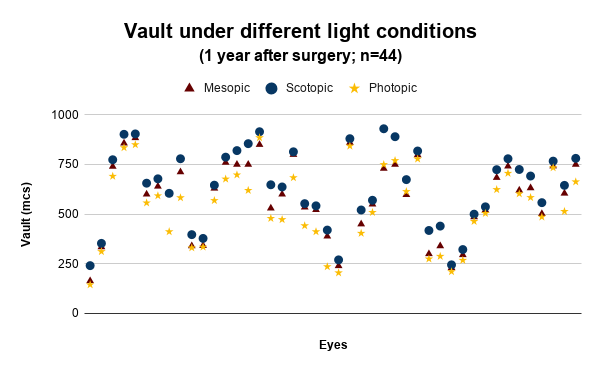
The mean vault measured with OCT under different lighting conditions is shown in figure 1, with the results for each eye, one year after surgery. Figure 2 shows the results obtained two years after surgery. Table 2 shows that a significant difference was not found when comparing vault values under different lighting conditions, one or two years after surgery. Figure 3 shows the results of differences in vault values between scotopic and photopic conditions (which represents how much the IPCL shifted due to a change in lighting intensity), one and two years after surgery. Regarding this information, in table 2 the statistical comparison can be observed, where significant differences between the first and second postoperative year results were found. In the same table, vault comparison between the first and second postoperative year for each lighting condition is also shown, which also did not show a statistical significant difference, expressing the stability of the ICPL vault through time.
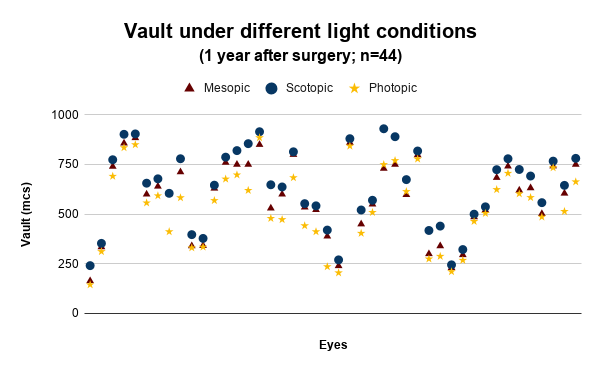
Figure 1. Vault measurements of a posterior chamber phakic lens IPCL V2.0, in mesopic, scotopic and photopic lighting conditions, one year after surgery.

Figure 2. Vault measurements of a posterior chamber phakic lens IPCL V2.0, in mesopic, scotopic and photopic lighting conditions, two years after surgery.

Figure 3. The difference between vault values of a posterior chamber phakic lens IPCL V2.0, comparing results of the scotopic versus the photopic lighting conditions, one and two years after surgery.
Table 1. Spherical equivalent, endothelial cell density and central corneal thickness evaluated in patients with posterior chamber phakic lens IPCL V2.0.
|
Preoperative |
1 year after surgery |
2 years after surgery |
p |
Spherical equivalent (D) |
-8.4 ± 3.5
(-3 to -17.1) |
-0,2 ± 0,3
(-1.3 to 0.6) |
-0.2 ±0.2
(-0.6 to 0.2) |
<0.001 |
Endothelial cell density (cells/mm2) |
2629.5 ± 219 (2135-3006) |
2548.6 ± 221.2
(2054-3006) |
2556.9 ± 203.4
(2136-3002) |
0.15 |
Central corneal thickness (mm) |
515.5 ± 35
(459-616) |
518.6 ± 36.8
(457-632) |
515 ± 28.7
(454-590) |
0.86 |
(D: dioptres).
Table 2. Comparison of the posterior chamber phakic lens IPCL V2.0 vault, between the first and second postoperative year for the different intensity of light conditions. In the last column is showed the statistical comparison between results obtained the first and second year. The result of the comparison between the scotopic versus photopic in each year is presented in the last file.
Vault (mm) |
1 year after surgery |
2 years after surgery |
p |
Mesopic conditions |
585.3 ± 192.1 (164-884) |
582.6 ± 192.4 (170-860) |
0.27 |
Scotopic conditions |
636.1 ± 196.9 (241-930) |
635.3 ± 240.5 (235-924) |
0.72 |
Photopic conditions |
536.7 ± 195.3 (145-885) |
536.9 ± 216 (142-1135) |
0.92 |
Shifting between scotopic and photopic conditions |
99.4 ± 52.3 (30-235)
p<0.001 |
98.4 ± 48.4 (27-239)
p<0.001 |
0.67 |
DISCUSSION
In this article we analyzed the first results obtained after performing anterior segment measurements, evaluating the posterior chamber phakic lens vault called IPCL V2.0, with its spherical, toric and diffractive models, one and two years after implantation. Measurements were performed at normal lighting conditions, and also at experimental controlled conditions (scotopic and photopic). The comparison between the obtained results for the first and the second postoperative year showed that the vault remained stable. Also, that the vault difference between the scotopic and the photopic lighting condition was slightly lower than 100 µm (99.4 µm and 98.4 µm, for the first and second years respectively), with represented a statistically significant difference, although cataracts did not develop. Another relevant result showed the improvement of the spherical equivalent improvement and the stability of the values of the endothelial cell density and central corneal thickness, where no statistical significant differences were found even two years after surgery.
The posterior chamber phakic lenses have shown safe and effective results, with only a few complications, such as the increase of intraocular pressure (which is absolutely infrequent with the new lens designs), pigment dispersion syndrome, halos perception and problems of lens rotation, and even lens dislocation. However, the development of cataracts is the main reason these lenses have been explanted21-22.
Regarding this aspect, and reviewing the published scientific evidence, even in the case of the ICL model, which is the posterior chamber phakic lens with the longest history (and, therefore, the lens with the largest amount of research studies and clinical experience), there is no uniformity of results. For example, Kocová H et al.5 published that, in a case-series of 62 eyes, lens opacity occurred in 18 eyes, which led to the explantation of the ICL lens in 7 eyes (11.3%) because vision was affected. Of those 7 eyes, 5 belonged to myopic patients, and 2 to hyperopes, with a mean follow up of 3.4 years old. The authors stated that they could not find a statistical correlation between the time that had elapsed after surgery and the development of cataracts, or of a lower vault. In regards to possible causes, they theorized that one case got uveitis, and the others were cataracts that developed in eyes with dislocated ICL lenses, in patients with a high level of myopia. Nevertheless, in the work published by Montes-Micó et al.22, where 35 related studies were reviewed, they found that cataract development was the most reported side effect, representing 0.17% of all of them. In that same review, however, they found a work published in 2015 (Alfonso et al.23), where a large series of 3420 cases of patients’ eyes was reviewed, with a wide range of ages (from 18 to 50 years old), and a wide range of preoperative spherical equivalents (from -26.5 to 12.5 D). In 21 eyes (0.61%) the ICL lens needed to be explanted due to cataract development, after a mean time of 4.2 years after surgery, in association with the patients’ age (higher risk at a higher age), and with higher levels of spherical equivalents.
Regarding cataracts development, it is clear that surgery must be performed without complications, prioritizing the care of the crystalline lens, and that having a complete, precise, and detailed preoperative knowledge of the anterior chamber anatomy is key when trying to select the adequate lens, not only in terms of its optical power, but also in regards to its size (diameter and thickness). Even though certain safety parameters regarding the preoperative “static” measures of the anterior chamber, and the postoperative obtained vault, were set, the importance of considering the dynamic characteristic of these parameters, related to pupil size and movement developed in the crystalline lens during the accommodation process, has recently been emphasized, as Gonzalez-Lopez et al. published in 201817. In their study, they conducted an experimental evaluation with low (0.5 LUX) and high (18500 LUX) light intensity in 39 eyes of myopic patients, using an anterior segment OCT and measuring different anterior chamber parameters, including the ICL vault values (from two models: Visian ICL V4c y EVO+). They found that in photopic conditions the mean vault was 374 ± 208 µm, whereas in scotopic conditions it increased to 540 ± 252 µm, generating a difference of 167 ± 70 µm. More parameters were measured and evaluated in this study, such as the diameter of the ICL lens (from 12.1 to 13.7 mm), its optical power (lower or higher than 10 D), the grade of miosis (according to the different pupil size, higher or lower than 3.3 mm).
In another study published by Kato et al.8, the vault was also evaluated under different lighting conditions, and they found a mean value of 476.1 ± 219.6 µm under photopic conditions, which grew to 521.1 ± 220 µm under scotopic conditions. In their experimental set-up, they considered the “scotopic” condition with a light intensity of 4 LUX, and 400 LUX for the photopic condition. The last one is equivalent to the light intensity used in the present work as “a mesopic condition”, which is the normal light condition used in the patient room. In a letter to the editor, Gonzalez-Lopez et al.24 mentioned that what they had done (0.5 LUX for scotopic conditions, and 18500 LUX for photopic conditions) was a better model that was closer to reality. Even though the set-up used in the present work uses a scotopic level similar to the one proposed by Gonzalez-Lopez et al., we could not reach the same lighting intensity for the photopic condition, and our photopic measurement was below that mark (1500 LUX). However, it was enough to notice miosis in the illuminated eye, which in turn led to miosis in the counter-lateral eye, due to consensual reflex.
There are others methodological differences in this present work regarding other published studies.
On one hand, we have added one more measurement (scotopic), considering it the “standard” lighting condition, which is the usual light intensity used in the patient room to perform routine postoperative OCT measurements, with the light turned-on, generating an intensity of 400 LUX, specifically at the level of the patient’s head (and eyes), verified by luxmeter measurements. On the other hand, while conducting the photopic evaluation, exposing the non-measured eye during 5 seconds to 1500 LUX, it was not occluded later, as Gonzalez-Lopez et al. did in their 2018 work17. Moreover, we think that the main difference is the device used to perform the measurements, because the OCT equipment was different. Furthermore, the evaluated lens was different, which could account in part for the differences that we found.
Therefore, taking into considerations the different methods previously mentioned, we can explain (in part) why the shifting vault in our study was lower than what was reported by Gonzalez-Lopez et al.17, and closer to the results published by Kato et al.18. It would be interesting to confirm with the IPCL V2.0 lens if we can maintain the same results with a higher lighting intensity, as was performed by Gonzalez-Lopez et al.17. One important aspect to point out is that the controlled and experimental lighting conditions evaluated in the present study are very close to real life situations that patients can encounter in their daily routine. For example, while driving at night on a dark route or street (scotopic condition), a driver can encounter another vehicle with high lights and be dazzled (photopic condition), which in turn could develop a vault shifting, with the potential risk of generating contact or touching the crystalline lens, regarding its vault measurements.
There are a few more things in regard to the results from the present series. Even though we did not detect neither cataracts nor corneal problems (this was confirmed by the stability of the endothelial cell density and the central corneal thickness), we have found cases with vault values lower than 250 µm (at a lower vault more, there is a greater risk of cataracts), and some cases with high vault values (over 900 µm), as seen in figures 1 and 2. Those cases are being followed more closely in order to rule-out any potential complications. However, it is interesting to point out that a series of recently published results showed that patients with low vault values with ICL lens had no complications, one year after surgery25. Similar results were obtained in the new work of Gonzalez-Lopez et al.26, with a follow up of four years, where they emphasized the importance of considering the dynamic nature of the phakic lens and the relevance of the central hole in the design of the this kind of lens, lowering the risk of cataract development in comparison with a previous ICL model. Anyway, these cases with low vaults must be followed through time. In our case series, the mean vault was high (582.6 µm), comparing with a recent publication developed with another phakic lens (ICL), where the mean vault was 486 µm22.
Finally, we must point out that this is the first study to date that has evaluated the IPCL V2.0 vault under different lighting conditions, which is the main strength of this article. As we have stated in the title, what we are showing here are preliminary results from a larger case series, where we will consider other parameters that have not yet been processed. We hope to obtain more information regarding possible connections after that, such as, for instance, if there are any differences in the IPCL diameter, the patients’ age, the anatomy of the anterior chamber and the obtained vault, under different lighting conditions, and in association with different pupil diameters. Additionally, we expect to determine, at least for this lens and with the device used to perform the measurements, if a new safety parameter can be added to the patient follow-up of with IPCL V2.0 lenses, considering the physiological movement of the crystalline lens.
CONCLUSIONS
After a two year follow-up, we observed that the posterior chamber phakic lens called IPCL V2.0 remained stable in its position. When the light intensity changed, we were able to register a shifting vault slightly lower than 100 µm. Even though no cataracts developed in any case after a two year follow-up, and the endothelial cell density and the central corneal thickness remained stable and within normal values, we will still need to continue studying and researching the anterior segment anatomy, considering dynamic conditions, and increasing the follow-up time of the cases, in order to potentially improve the indications criteria and the preoperative selections of patients, as well as reducing postoperative complications.
REFERENCES
1. Kamiya K, Shimizu K, Igarashi A et al. Posterior chamber phakic intraocular lens implantation: comparative, multicentre study in 351 eyes with low-to-moderate or high myopia. Br J Ophthalmol 2018; 102: 177-181.
2. Choi JH, Lim DH, Nam SW et al. Ten-year clinical outcomes after implantation of a posterior chamber phakic intraocular lens for myopia. J Cataract Refract Surg 2019; 45: 1555-1561.
3. Vargas V, Alió JL, Barraquer RI et al. Safety and visual outcomes following posterior chamber phakic intraocular lens bilensectomy. Eye Vis (Lond) 2020; 7: 34.
4. Kobashi H, Kamiya K, Igarashi A et al. Long-term quality of life after posterior chamber phakic intraocular lens implantation and after wavefront-guided laser in situ keratomileusis for myopia. J Cataract Refract Surg 2014; 40: 2019-2024.
5. Kocová H, Vlková E, Michalcová L et al. Incidence of cataract following implantation of a posterior-chamber phakic lens ICL (Implantable Collamer Lens): long-term results. Cesk Slov Oftalmol 2017; 73: 87-93.
6. Nakamura T, Isogai N, Kojima T et al. Posterior chamber phakic intraocular lens implantation for the correction of myopia and myopic astigmatism: a retrospective 10-year follow-up study. Am J Ophthalmol 2019; 206: 1-10.
7. Hayakawa H, Kamiya K, Ando W et al. Etiology and outcomes of current posterior chamber phakic intraocular lens extraction. Sci Rep 2020; 10: 21686.
8. Kohnen T, LaFontaine L, Andrew R; Study Investigators. Long-term safety follow-up of an anterior chamber angle-supported phakic intraocular lens. J Cataract Refract Surg 2017; 43: 1163-1170.
9. Jonker SMR, Berendschot TTJM, Ronden AE et al. Long-term endothelial cell loss in patients with Artisan myopia and Artisan toric phakic intraocular lenses: 5- and 10-year results. Ophthalmology 2018; 125: 486-494.
10. Vargas V, Alio JL. Refractive outcomes and complications following angle supported, iris fixated, and posterior chamber phakic intraocular lenses bilensectomy. Curr Opin Ophthalmol 2021; 32: 25-30.
11. Mastromonaco C, Balazsi M, Saheb N et al. Histopathological changes in the anterior segment with anterior and posterior chamber intraocular lens. Can J Ophthalmol 2020; 55: 437-444.
12. Vasavada V, Srivastava S, Vasavada SA et al. Safety and efficacy of a new phakic posterior chamber IOL for correction of myopia: 3 years of follow-up. J Refract Surg 2018; 34: 817-823.
13. Sachdev G, Ramamurthy D. Long-term safety of posterior chamber implantable phakic contact lens for the correction of myopia. Clin Ophthalmol 2019; 13: 137-142.
14. Bianchi GR. Initial results from a new model of posterior chamber implantable phakic contact lens: IPCL V2.0. Med Hypothesis Discov Innov Ophthalmol 2019; 8: 57-63.
15. Bianchi GR. Presbyopia management with diffractive phakic posterior chamber IOL. Cesk Slov Oftalmol 2020; 76: 211-219.
16. Petternel V, Köppl CM, Dejaco-Ruhswurm I et al. Effect of accommodation and pupil size on the movement of a posterior chamber lens in the phakic eye. Ophthalmology 2004; 111: 325-331.
17. González-López F, Mompean B, Bilbao-Calabuig R et al. Dynamic assessment of light-induced vaulting changes of implantable collamer lens with central port by wwept-source OCT: pilot study. Transl Vis Sci Technol 2018; 7: 4.
18. Kato S, Shimizu K, Igarashi A. Vault changes caused by light-induced pupil constriction and accommodation in eyes with an implantable collamer lens. Cornea 2019; 38: 217-220.
19. Cerpa Manito S, Sánchez Trancón A, Torrado Sierra O et al. Inter-eye vault differences of implantable collamer lens measured using anterior segment optical coherence tomography. Clin Ophthalmol 2020; 14: 3563-3573.
20. Gargallo-Martínez B, García-Medina JJ, Rubio-Velázquez E et al. Vault changes after cyclopentolate instillation in eyes with posterior chamber phakic intraocular lens. Sci Rep 2020; 10: 9646.
21. Tang Y, Ye J. Phakic posterior chamber intraocular lens with a central hole in treating patients with moderate to high myopia: a meta-analysis. J Ophthalmol 2019; 2019: 9496326.
22. Montes-Micó R, Ruiz-Mesa R, Rodríguez-Prats JL, Tañá-Rivero P. Posterior-chamber phakic implantable collamer lenses with a central port: a review. Acta Ophthalmol 2020 Aug 25. doi: 10.1111/aos.14599.
23. Alfonso JF, Lisa C, Fernández-Vega L et al. Prevalence of cataract after collagen copolymer phakic intraocular lens implantation for myopia, hyperopia, and astigmatism. J Cataract Refract Surg 2015; 41: 800-805.
24. González-López F, Mompean B, Bilbao-Calabuig R et al. Response to “Vault changes caused by light-induced pupil constriction and accommodation in eyes with an implantable collamer lens”. Cornea 2019; 38: e36-e37.
25. Kato S, Shimizu K, Igarashi A. Assessment of low-vault cases with an implantable collamer lens. PLoS One 2020; 15: e0241814.
26. González-López F, Bouza-Miguens C, Tejerina V et al. Long-term assessment of crystalline lens transparency in eyes implanted with a central-hole phakic collamer lens developing low postoperative vault. J Cataract Refract Surg 2021; 42: 204-210.