CLINICAL CASES
Eyes can remain healthy after 40 years of an anterior chamber intraocular lens
Christian Le Roy Marza, Miguel Ángel Ibáñez Hernándeza, Arturo Iván Pérez Pachecob
a Departamento de Investigación, Catarata y Cirugía Refractiva, Hospital Puerta de Hierro, Jalisco, México.
b Departamento de Investigación, Catarata y Cirugía Refractiva, Hospital Star Médica, Querétaro, México.
Received: April 3rd, 2025.
Approved: May 26th, 2025.
Corresponsal author
Dr. Arturo Iván Pérez Pacheco
Departamento de Investigación, Catarata y Cirugía Refractiva
Hospital Star Médica, Querétaro, México.
+52 (442) 356 65 81
arturo.perez.pacheco473@gmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2025; 18(2): e229-e235.
https://doi.org/10.70313/2718.7446.v18.n2.425
Conflict of interest
The authors declare that they have no conflicts of interest.
Abstract
Objective: To present the case of a patient with an anterior chamber intraocular lens (AC-IOL) for 40 years, with no complications, highlighting that when the patient’s indication is appropriate, they are safe implants.
Case report: We present an 85-year-old woman who comes to ophthalmology department for an evaluation for a comprehensive visual health check and with the presence of hyposphagma in the right eye (RE). As a relevant data, we found that extracapsular cataract extraction was performed in the RE, with placement of a posterior chamber. In the contralateral eye left eye (LE), intracapsular cataract extraction was done, with an AC-IOL implanted, with more than 40 years ago. The physical examination assessed visual acuity of 20/100 RE and 20/80 LE. Best-corrected visual acuity 20/50 RE and 20/40 LE. Pachymetry of RE 526 microns and LE 538 microns, intraocular pressure of 15 mmHg RE, and 16 mmHg LE. RE refraction: -4.00 -3.75 177° and LE -6.50 -2.75 50°. Endothelial cell density was 1786 cells/mm2 and 2552 cells/mm2 (RE, LE respectively). Pleomorphism and polymegatism were both normal in each eye.
Conclusion: This case represents that if the patient is chosen correctly, the implantation of an anterior chamber IOL can give good anatomical and functional results without complications, even 40 years after surgery.
Keywords: anterior chamber intraocular lens, intracapsular cataract extraction, endothelial microscopy, refraction, visual quality.
Los ojos pueden permanecer sanos después de 40 años de una lente de cámara anterior
Resumen
Objetivo: Presentar el caso de un paciente con una lente intraocular de cámara anterior (LIO-CA) durante 40 años, sin complicaciones, destacando que cuando la indicación del paciente es adecuada, son implantes seguros.
Caso clínico: Presentamos el caso de una mujer de 85 años de edad que acudió al servicio de oftalmología para valoración de salud visual general y por presencia de hiposfagma en ojo derecho (OD). Como datos relevantes, encontramos que en el ojo derecho (OD) se había realizado una extracción de catarata extracapsular en el pasado, con colocación de una LIO de cámara posterior; en el ojo izquierdo (OI) se había realizado extracción de catarata intracapsular, con implante de una LIO-CA con más de 40 años de antigüedad. En la exploración física se encontró una agudeza visual de 20/100 OD y 20/80 OI. Agudeza visual mejor corregida de 20/50 RE y 20/40 LE. Paquimetría de 526 micras en OD y 538 micras en OI, presión intraocular de 15 mmHg en OD y 16 mmHg en OI. Refracción OD: -4,00 -3,75 177° y OI -6,50 -2,75 50°. La densidad de células endoteliales era en el OD de 1786 células/mm2 y 2552 células/mm2 en el OI. El pleomorfismo y el polimegatismo fueron normales en cada ojo.
Conclusiones: Este caso representa que si el paciente es elegido correctamente, el implante de una LIO de cámara anterior puede dar buenos resultados anatómicos y funcionales sin complicaciones, incluso 40 años después de la cirugía.
Palabras clave: lente intraocular de cámara anterior, extracción intracapsular de cataratas, microscopía endotelial, refracción, calidad visual.
Os olhos podem permanecer saudáveis 40 anos após a substituição da lente da câmara anterior
Resumo
Objetivo: Apresentar o caso de um paciente portador de lente intraocular de câmara anterior (LIO-CA) há 40 anos, sem complicações, ressaltando que quando a indicação do paciente é adequada, os implantes são seguros.
Caso clínico: Apresentamos o caso de uma mulher de 85 anos que se compareceu ao departamento de oftalmologia para avaliação geral da saúde visual e a presença de hiposfagma no olho direito (OD). Dados relevantes incluíram a extração prévia de catarata extracapsular no olho direito (OD), com colocação de uma LIO de câmara posterior; o olho esquerdo (OE), com o implante de uma LIO intracapsular de catarata com mais de 40 anos, havia sido realizado. O exame físico revelou acuidade visual de 20/100 OD e 20/80 OE. A acuidade visual melhor corrigida foi de 20/50 OD e 20/40 OE. A paquimetria foi de 526 mícrons no OD e 538 mícrons no OE, e a pressão intraocular foi de 15 mmHg no OD e 16 mmHg no OE. Refração OD: -4,00 -3,75 177° e OE: -6,50 -2,75 50°. A densidade de células endoteliais era de 1.786 células/mm² no olho direito e 2.552 células/mm² no OE. Pleomorfismo e polimegatismo eram normais em ambos os olhos.
Conclusões: Este caso demonstra que, se o paciente for adequadamente selecionado, o implante de uma LIO de câmara anterior pode produzir bons resultados anatômicos e funcionais sem complicações, mesmo 40 anos após a cirurgia.
Palavras-chave: lente intraocular de câmara anterior, extração de catarata intracapsular, microscopia endotelial, refração, qualidade visual.
Introduction
Many years ago, just before intraocular lenses were invented, patients had to get used to wearing thick and heavy crown glass spectacles or uncomfortable contact lenses, after cataract removal secondary to aphakic hypermetropia1.
However, it wasn’t until the 1950s that intraocular lenses became popular after Dr. Harold Rydley implanted the first polymethyl methacrylate (PMMA) posterior chamber (PC) bag intraocular lens (IOL), resembling the natural eye lens2. By this time, the most important complication was IOL’s dislocation, due to the overweight and poor anchor capacities, without ceasing to mention, of course, the refractive surprises over +18.0 diopters1-2.
With the passage of time and the advent of new technologies, different models started to emerge, including anterior chamber IOLs (AC-IOL), with physical conformations and designs with different optics and haptics3. Such is the case that many ophthalmologists preferred AC-IOLs over PC-IOLs, because they could be easily implanted after extracapsular cataract extraction (EECC) and intracapsular cataract extraction (IECC), and no capsular support was needed. Nevertheless, the complications with AC-IOLs started to emerge, including the most feared, endothelial cell loss, corneal decompensation, and any pupillary-associated difficulty3-5.
At first, there was no clear understanding of the reason or association of the complication, however complications were later associated with the lens vault, which first generations of AC-IOLs were not really calculated and therefore very close to the endothelium, bringing consequently an abnormal flow of the aqueous humor, inducing endothelial damage and corneal failure at the end3-4. On the other hand, iridocorneal synechiae and chronic inflammation due to angle-supported haptics were also reported, producing severe secondary glaucoma after a short period3-5.
Unfortunately for the above reasons, a lot of AC-IOLs had to be later explanted due to severe sight-threatening complications; so, it became necessary iridectomies, because of several reports of pupillary blocking5. Over time, the ophthalmological industry began the design and creation of new lenses, using new materials, with better efficiency of shape and sizes, which allowed the non-interaction with the endothelium and thus respecting the natural anatomy of the eye. In this context, our objective is to present a case where we found a patient with an AC-IOLs for the last 40 years, with no secondary alterations, in order to highlight that when the patient’s indication is appropriate, these implants are effective and safe.
Case report
We present a 85-year-old woman who came to the ophthalmology department for an evaluation, for a comprehensive visual health check with the presence of hyposphagma in the right eye (RE).
As a relevant personal pathological history we found that EECC surgery was performed in the RE, with placement of a PC-IOL. In the contralateral eye left eye (LE), IECC technique surgery was done, with an anterior chamber IOL implanted, with more than 40 years ago.
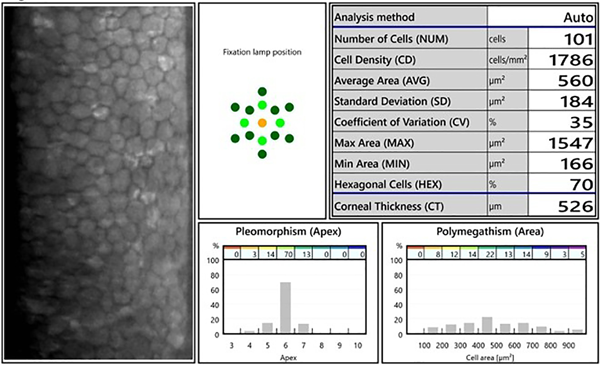
The physical examination assessed visual acuity (VA) of 20/100 RE and 20/80 LE. Best-corrected visual acuity (BSCVA) 20/50 RE and 20/40 LE. Pachymetry of RE 526 microns and LE 538 microns, intraocular pressure (IOP) of 15 RE AND 16 LE. RE refraction: SpH -4.00 CyL -3.75 x 177° and LE SpH -6.50 CyL -2.75 x 50°. Endothelial cell count was in the RE 1786 cells and 2552 cells respectively. Pleomorphism and Polymegatism were both normal in each eye (Figs. 1 & 2).
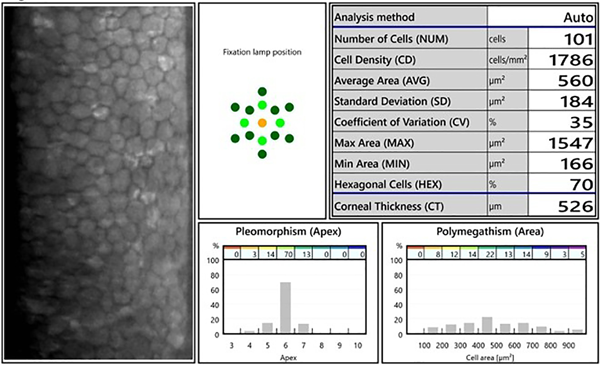
Figure 1. Endothelial microscopy of the right eye.
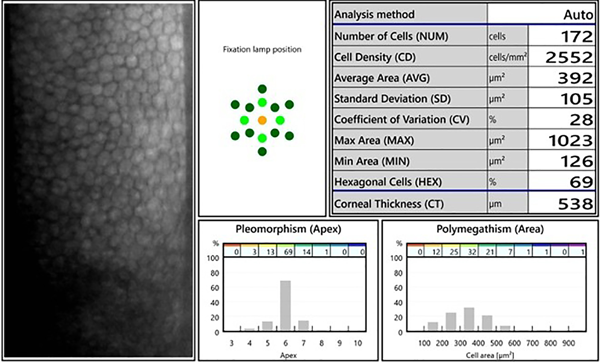
Figure 2. Endothelial microscopy of the left eye.
With biomicroscopy examination of the anterior segment LE, it was observed with adequate implantation of eyelashes, without eyelid alterations, without signs of infection, conjunctiva and sclera with hyposphagma in resolution, transparent cornea, formed anterior chamber, 5-piece AC-IOL, centered, without endothelial touch, superior iridectomy in the meridian of 12. On the other hand, the Adelphi eye was found unaltered. In both eyes, an attached retina with typical high myopia changes was found, and no further lesions were presented (Fig. 3). The optical quality of both eyes, despite the different characteristics of endothelial microscopy and the type of surgery and intraocular lens implantation, show stability and satisfaction in the patient (Fig. 4).
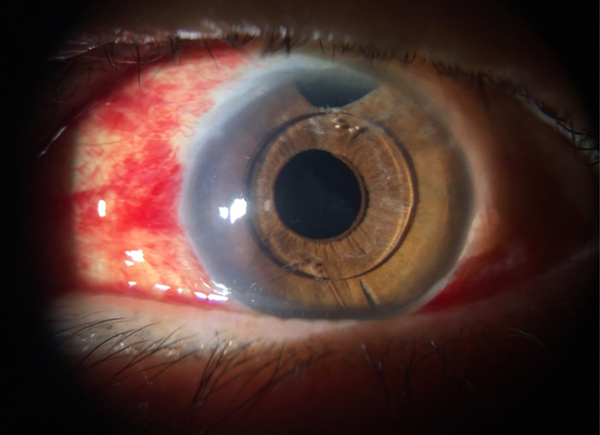
Figure 3. Anterior segment of the left eye is observed with hyposphagnum in resolution, with AC IOL and upper central iridotomy.
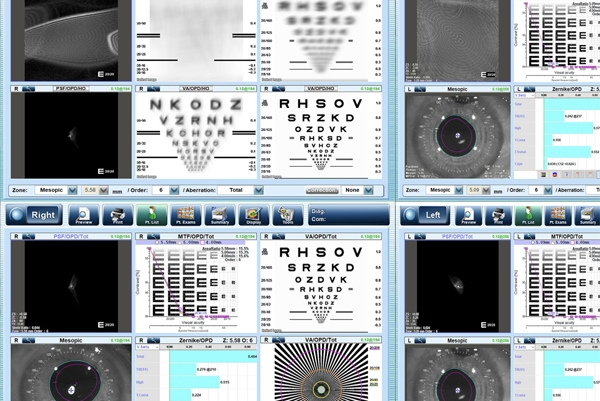
Figure 4. Optical quality represented in both eyes.
Discussion
It is not an everyday experience to examine a patient due to hyposfagma and realize the eye is in good health condition after 40 years of AC-IOL.
We want to focus special attention on the left eye because of the current health status despite 40 years of AC-IOL implantation. This case represents quite the opposite of many reports of failed implantation of AC-IOLs in particular those from first generations6-7.
Although AC IOLs have been found to improve visual acuity, corneal endothelial cell loss is a common long-term complication3-5, these lenses have also been implicated in several other unwanted results, such as corneal decompensation, increase in IOP, pupillary distortion, cystoid macular edema and even retinal detachment9.
We have to consider that this kind of AC-IOLs (5-piece angle supported IOLs) was suspended in many 1st world countries due to poor quality results and several complications. These lenses were later exported to underdeveloped countries and implanted for many further years. This was probably the circumstance of this case. For many surgeons, these kinds of lenses were the only options available at that time.
This case represents long-term implantation of aphakic anterior chamber IOL with excellent results, comparable to other studies such as a prospective studies by Droslum in which 18 of 20 aphakic eyes had acceptable results after 6 to 8 years follow up8. This indicates that anterior chamber IOLs can be safe in selected patients. It may seem that the proximity of anterior chamber IOLs to the cornea represents a higher endothelial loss, mostly seen in first-generation models, such as the Leiske, which had a corneal decompensation rate of 8.4 after 12.9 years, seen by Panton et al.9.
Although new aphakic AC-IOLs have emerged such as the Artisan Iris Claw, open loop AC IOL, Kellman multiflex IOL, and MTA3UO AC IOLs they are still related, in different degrees, to complications. Newer techniques like scleral fixated IOLs or posterior iris claw lenses have demonstrated good follow-up results regarding endothelial cell loss10-11, although the learning curve is higher in these techniques and vitrectomy is necessary in most cases. In a study driven by Ellerton et al., only 1 of 81 cases of flexible, open-loop anterior chamber IOLs developed bullous keratopathy after 30 months12. However, authors like Droslum conclude that anterior chamber IOLs can be well tolerated if there is a lack of preexisting corneal pathology8, and the case we have presented could be an example of this.
Conclusion
In summary, this case represents that if the patient is chosen correctly, the implantation of an anterior chamber IOL can give good anatomical and functional results without complications, even 40 years after surgery.
References
1. Olson RJ. Cataract Surgery from 1918 to the present and future-just imagine! Am J Ophthalmol 2018; 185: 10-13. doi:10.1016/j.ajo.2017.08.020.
2. Ridley H. Intra-ocular acrylic lenses after cataract extraction 1952. Bull World Health Organ 2003; 81(10): 758-761.
3. Moschos MM, Nitoda E. The correction of aphakia using anterior chamber intraocular lens. In Vivo 2016; 30(6): 733-738. doi:10.21873/invivo.10988.
4. Güell JL, Morral M, Kook D, Kohnen T. Phakic intraocular lenses part 1: historical overview, current models, selection criteria, and surgical techniques. J Cataract Refract Surg 2010; 36(11): 1976-1993. doi:10.1016/j.jcrs.2010.08.014.
5. Ardjomand N, Kölli H, Vidic B, El-Shabrawi Y, Faulborn J. Pupillary block after phakic anterior chamber intraocular lens implantation. J Cataract Refract Surg 2002; 28(6): 1080-1081. doi:10.1016/s0886-3350(01)01114-2.
6. Allemann N, Chamon W, Tanaka HM et al. Myopic angle-supported intraocular lenses: two-year follow-up. Ophthalmology 2000; 107(8): 1549-1554. doi:10.1016/s0161-6420(00)00221-9.
7. Oakley CL, Nigro MA, Vote BJ. Fifty-year follow-up and Strampelli anterior chamber intraocular lens. GMS Ophthalmol Cases 2015; 5: Doc06. doi:10.3205/oc000028.
8. Drolsum L. Long-term follow-up of secondary flexible, open-loop, anterior chamber intraocular lenses. J Cataract Refract Surg 2003; 29(3): 498-503. doi:10.1016/s0886-3350(02)01614-0.
9. Panton RW, Viana MG, Panton PJ, Panton JH. Long-term follow-up of leiske closed-loop anterior chamber intraocular lenses. J Cataract Refract Surg 2000; 26(4): 590-596. doi:10.1016/s0886-3350(99)00398-3.
10. Zhao H, Wang W, Hu Z, Chen B. Long-term outcome of scleral-fixated intraocular lens implantation without conjunctival peritomies and sclerotomy in ocular trauma patients. BMC Ophthalmol 2019; 19(1): 164. doi:10.1186/s12886-019-1172-4.
11. Kandemir Beşek N, Alagoz N, Gumus G et al. Long-term results of aphakia management by scleral fixation intraocular lens placement with knotless transscleral Z-suture method. Int Ophthalmol 2020; 40(6): 1449-1454. doi:10.1007/s10792-020-01311-w.
12. Ellerton CR, Rattigan SM, Chapman FM, Chitkara DK, Smerdon DL. Secondary implantation of open-loop, flexible, anterior chamber intraocular lenses. J Cataract Refract Surg 1996; 22(7): 951-954. doi:10.1016/s0886-3350(96)80197-0.