SURGICAL TECHNIQUES AND DIAGNOSTIC METHODS
Hyaloid pupillary seclusion: anterior hyaloidectomy in the retroiridian chamber. A novel technique for acute closed-angle glaucoma secondary to post-traumatic pupillary block due to herniation of the vitreous body with an intact hyaloid membrane
Andrés Germán Alza
Clínica Privada de Ojos Dr. Enrique Alza, La Plata (Buenos Aires), Argentina.
Received: March 13st, 2025.
Approved: May 10th, 2025.
Contact
Dr. Andrés Germán Alza
Clínica Privada de Ojos Dr. Enrique Alza
Calle 12, nro. 662
(1900) La Plata, provincia de Buenos Aires
Argentina
+ 54 9 221 4219682
andresalza@hotmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2025; 18(2): e243-e251.
https://doi.org/10.70313/2718.7446.v18.n2.412
Abstract
We present an unusual case of pupillary vitreous herniation with an intact hyaloid membrane, associated with anterior dislocation of the intraocular lens, an intact capsular bag, and a partially intact zonule. This case occurred in an 85-year-old patient with acute post-traumatic glaucoma immediately following cataract surgery. In the absence of similar reports, an innovative surgical technique was proposed: anterior hyaloidectomy in the retroiridian chamber. This minimally invasive procedure, performed by peripheral iridectomy, includes prelental anterior retroiridian vitrectomy, facilitating spontaneous repositioning of the intraocular prosthesis. The visual and anatomical results were favorable, demonstrating the potential efficacy of this technique for anterior segment surgeons.
Keywords: acute glaucoma, pupillary block, cataract, anterior lens luxation, hyaloid.
Introduction
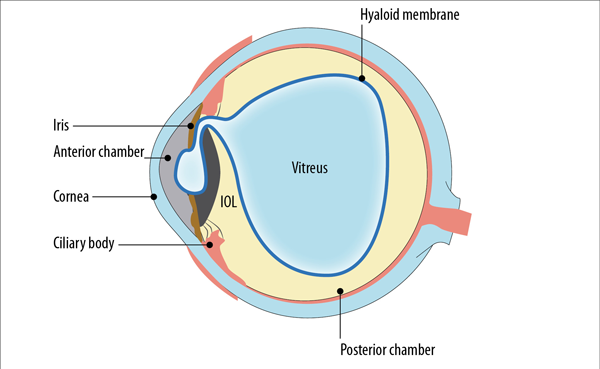
We report a rare case of vitreous herniation with an intact hyaloid membrane into the anterior and retroiridian chambers, resulting in pupillary seclusion due to entrapment, and associated with anterior intraocular lens (IOL) dislocation within an intact capsular bag and a partial intact zonule (Fig. 1). The goal of treatment is to restore normal aqueous flow and anterior segment anatomy. Although peripheral iridotomy with an Nd:YAG laser is the initial procedure of choice for similar cases, it is often difficult or insufficient, requiring a complementary vitrectomy. Therefore, we propose a novel technique: anterior hyaloidectomy in the retroiridian chamber. The procedure is performed through a minimal peripheral iridectomy within the retroiridian chamber associated with spontaneous repositioning of the IOL, taking advantage of the corneal incisions from the previous surgery and thus avoiding the need for a classic pars plana vitrectomy with its associated complications.
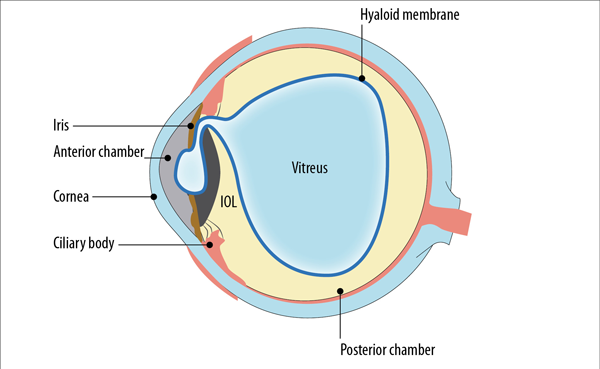
Figure 1. Vitreous herniation with an intact hyaloid membrane into the anterior and retroiridian chambers, resulting in pupillary seclusion due to entrapment, and associated with IOL dislocation within an intact capsular bag and a partial intact zonule.
Case
We present the case of an 85-year-old man who underwent cataract surgery in the right eye (RO) in November 2024. A foldable, monofocal, hydrophilic acrylic IOL (S-Lens, Sidapharm) was implanted without apparent complications.
Seventy-two hours after the procedure, the patient presented to the emergency department complaining of sudden vision loss following ocular trauma due to scratching. Slit-lamp biomicroscopy (SLM) using the Van Herick technique revealed a narrowed anterior chamber with angle block (Fig. 2A). Direct illumination with the optical section detected pupillary seclusion associated with vitreous opacity in the form of a “recumbent parabola” reflex corresponding to the intact anterior hyaloid surface herniated into the anterior chamber (Fig. 2B). The vitreous acts as a magnifying glass, denoting false posterior displacement of the IOL. Ocular pressure monitoring with a Goldmann tonometer yielded values greater than 60 mmHg.
Additional studies were performed, and previous studies were analyzed for a detailed evaluation. A Scheimpflug (SC) camera revealed a preserved anterior segment prior to cataract surgery (Fig. 3A). Seventy-two hours after the trauma, narrowing of the anterior chamber and pupillary vitreous was observed (Fig. 3B), and postoperatively, the anterior chamber deepened again, restoring the anterior segment anatomy (Fig. 3C). Optical coherence tomography (OCT) examination revealed narrowing of the anterior chamber, pupillary block, and the presence of an intact anterior hyaloid membrane with anterior displacement of the IOL, possibly due to rotation of the ciliary processes, resulting in an anterior chamber depth (ACD) of approximately 2313 mm (Fig. 4A). Angular block also occurred with iris incarceration in the incision (Fig. 4B and C). Ocular response analysis (ORA) of the OD revealed altered corneal hysteresis due to the cornea’s inability to absorb and dissipate energy due to elevated intraocular pressure and corneal edema (Fig. 5).
Based on these findings and given that we have not found any similar cases in the literature, we interpret the condition as a herniation of the vitreous body with the hyaloid intact into the anterior and retroiridian chambers, blocking the pupil due to entrapment, together with forward dislocation of the IOL, contained in the bag and with a partially intact zonule. Therefore, an innovative surgical technique called anterior hyaloidectomy of the retroiridian chamber was performed, with spontaneous repositioning of the IOL. At 10 days postoperatively, SLM showed a round pupil, iris released from the incision and peripheral iridectomy with deepening of the anterior chamber and positioned IOL (Fig. 2C and D) resulting in a visual improvement to LogMAR 0. Complementary examinations such as SC (Fig. 3C) and OCT (Fig. 6) corroborated these results, validating the success of the surgical procedure.

Figure 2. Images obtained using the OCUFY® WIDE device, illustrating the case’s progression. (A) and (B) show findings of 72 hours post-ocular trauma, including decreased anterior chamber depth with angle closure and the presence of vitreous opacity in the form of a “recumbent parabola” reflex corresponding to the intact anterior hyaloid surface herniated into the anterior chamber. (C) and (D) show improvement 10 days postoperatively, with deepened anterior chamber, round pupil, released iris, and the presence of a temporal peripheral iridectomy.
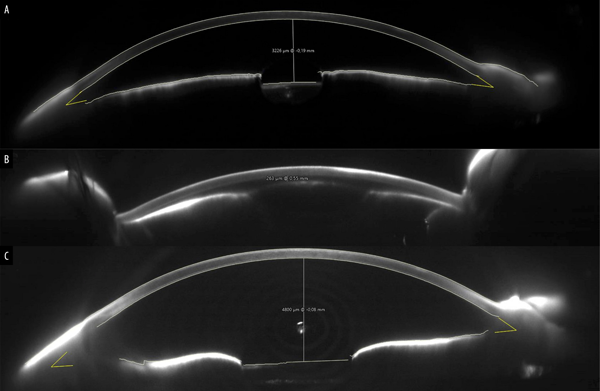
Figure 3. Demonstrates the evolution of the patient's anterior segment using SC. Initially (A), a preserved anterior segment was observed before cataract surgery. Following the trauma (B), narrowing of the anterior chamber and pupillary vitreous haze were evident. Post retroiridian anterior hyaloidectomy (C), the restoration of the anterior segment anatomy with deepening of the anterior chamber.
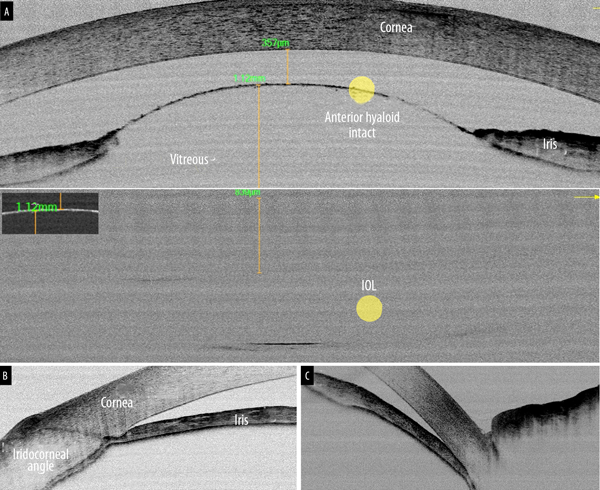
Figure 4. OCT at 72 hours post-trauma: revealed narrowing of the anterior chamber and presence of an intact anterior hyaloid membrane with displacement of the IOL towards the posterior chamber (A). In addition, angular block (B), with iris incarceration will be observed in incisions (C).

Figure 5. ORA of the OD, showed a significant alteration of the corneal hysteresis due to the inability of the cornea to absorb and dissipate energy due to high intraocular pressure.
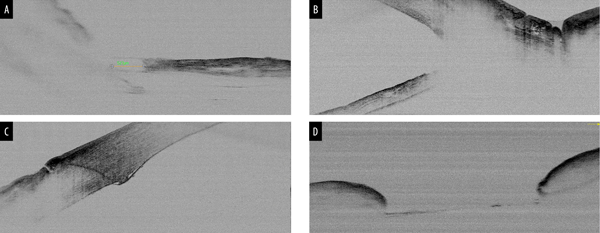
Figure 6. OCT at 72 hours post-trauma: narrowing of the anterior chamber, pupillary block and presence of the intact anterior hyaloid, with anterior displacement of the IOL (A). In addition, iris incarceration in the incision (B), with angular block (C).
Surgical technique
The following steps were performed (Table 1):
1. Intracameral anaesthesia was administered using a spatulated cannula, with a mixture of 0.75 ml of preservative-free 1% lidocaine and 0.75 ml of Ringer lactate.
2. Patient with seclusion glaucoma prior to surgery (Fig. 7A).
3. Surgery was initiated using the two incisions, primary and secondary, previously created during cataract surgery 72 hours prior. The main and secondary incisions were rescued with the same handpieces.
4. Small-diameter temporal peripheral iridectomy was performed with Wescott scissors and 0.12 mm serrated Castroviejo forceps (Fig. 7B).
5. Entry into the anterior chamber was made through the secondary incision with the continuous irrigation handpiece (Fig. 7C).
6. Anterior vitrectomy was performed with a 20 G gauge through the primary incision, threading through the iridotomy and accessing the retroiridian chamber. The following parameters were used: cutting speed of 1000 cpm, aspiration rate of 20 cc/min and vacuum of 250 mmHg (Fig. 7C).
7. Patient after retroiridian anterior hyaloidectomy through the peripheral iridectomy (Fig. 7D).
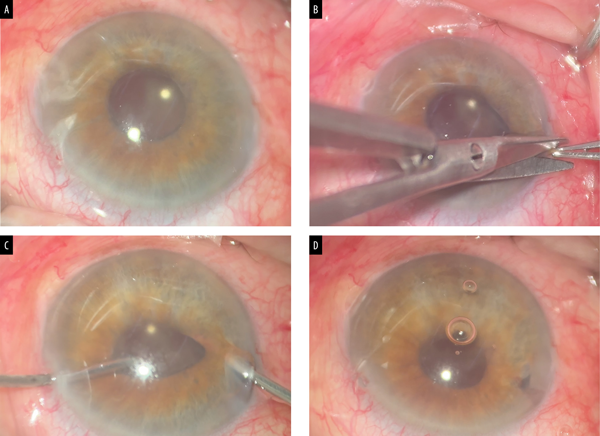
Figure 7. Patient with seclusion glaucoma before surgery (A). Small diameter peripheral temporal iridectomy was performed using Wescott scissors and 0.12 mm serrated Castroviejo forceps (B). The anterior chamber was entered through the secondary incision with the continuous irrigation handpiece. An anterior vitrectomy was performed through the primary incision, threading through the iridotomy and accessing the retroiridian chamber (C). Patient after anterior hyaloidectomy retroiridian through peripheral iridectomy (D).
Table 1. The following steps were performed.
STEP |
PROCEDURE |
1 |
Administration of intracameral anaesthesia (0.75 ml 1% lidocaine preservative-free + 0.75 ml Ringer’s lactate) using a spatula-tipped cannula. |
2 |
Re-opening of primary and secondary incisions (created 72 hours prior during cataract surgery) using the same handpieces. |
3 |
Small diameter temporal peripheral iridectomy using Wescott scissors and 0.12 mm Castroviejo serrated forceps. |
4 |
Entry into the anterior chamber through the secondary incision using a continuous irrigation handpiece. |
5 |
Anterior vitrectomy (20G) through the primary incision, accessing the retroiridian space via the iridectomy. Parameters: cut rate 1000 cpm, aspiration 20 cc/min, vacuum 250 mmHg. |
Discussion
Due to the absence of cases reported in the literature, we present a case of acute post-traumatic glaucoma resulting from pupillary entrapment of a vitreous hernia with an intact hyaloid membrane associated with anterior dislocation of the IOL within an intact capsular bag and partially preserved zonula.
An innovative surgical technique is proposed: anterior hyaloidectomy of the retroiridian chamber. This procedure consists of a peripheral iridectomy, followed by an anterior hyaloidectomy and a prelental anterior retroiridian vitrectomy. The technique facilitates spontaneous IOL repositioning and can be performed by anterior segment surgeons.
The retroiridian chamber, delimited by the posterior surface of the iris, ciliary muscle, ciliary processes, zonule, and anterior lens, is crucial for aqueous humor dynamics1. Vitreorrhagia in this space associated with trauma may involve the hyaloid membrane, as in our case, or the vitreous humor2. Traditionally, pars plana vitrectomy is the treatment of choice in similar cases; therefore, a novel surgical alternative is proposed for this case.
To contextualize this proposal, it is essential to review the concepts of malignant glaucoma (Von Graefe, 1869) and pupillary seclusion, both related to aqueous outflow disturbances (Table 2). In malignant glaucoma, techniques such as anterior capsulohyaloidectomy with anterior vitrectomy have been described3-4.
This innovative technique represents a safe and effective alternative in these complex cases. It is crucial to differentiate this technique from retroiridian anterior vitrectomy for the removal of late cortical remnants located in the posterior segment for anterior segment surgeons5. It is crucial to differentiate this technique from retroiridian anterior vitrectomy for the removal of late cortical remnants involving the posterior segment5.
Studies with larger caseloads and longer follow-up are needed to validate its long-term efficacy.
Table 2. Comparison between malignant glaucoma and pupillary seclusion.
CHARACTERISTIC |
MALIGNANT GLAUCOMA |
PUPILLARY SECLUSION |
Background |
Can occur post-surgery. |
Can occur post-surgery. |
Cause |
Ciliary block and misdirection of aqueous. |
Pupillary block and accumulation of aqueous humour. |
Angle-closure mechanism |
Misdirection of aqueous into the vitreous, pushing the lens and iris forward. |
Pupil block that pushes the iris forward due to the accumulation of aqueous humour. |
Synechiae |
Not always present. |
Always present. |
Treatment |
Reverse the misdirection of aqueous. |
Break the block to re-establish aqueous flow. |
Conclusion
Anterior hyaloidectomy of the retroiridian chamber is presented as an innovative surgical technique for the treatment of acute angle-closure glaucoma secondary to post-traumatic pupillary block of the intact anterior hyaloid in the acute phase. This procedure offers a less invasive alternative to pars plana vitrectomy, with favorable visual and anatomical results in the presented case. However, studies with larger caseloads and longer follow-up are required to validate its long-term efficacy and safety. Standardization of this technique could represent an advance in the management of this complex ophthalmological condition.
References
1. Alza AG. Staining with trypan blue and retroiridian synechiolysis: effective approach in cataract surgery for patients with chronic uveitis, severe miosis, and posterior synechiae. Oftalmol Clin Exp 2024; 17(3): e464-e472. doi:10.70313/2718.7446.v17.n03.358
2. Arriola-Villalobos P, Iglesias-Lodares I, Díaz-Valle D, Garcia-Gil-de-Bernabé J. Glaucoma agudo por bloqueo pupilar secundario a luxación posterior de lente acrílica intraocular tras capsulotomía Nd:YAG. Arch Soc Esp Oftalmol 2011; 86(9): 300-302. doi:10.1016/j.oftal.2011.04.014.
3. Basgil Pasaoglu I, Altan C, Bayraktar S, Satana B, Basarır B. Surgical management of pseudophakic malignant glaucoma via anterior segment-peripheral iridectomy capsulo-hyaloidectomy and anterior vitrectomy. Case Rep Ophthalmol Med 2012; 2012: 794938. doi:10.1155/2012/794938. Errata corrected in Case Rep Ophthalmol Med 2013; 2013: 940497. doi: 10.1155/2013/940497.
4. Żarnowski T, Wilkos-Kuc A, Tulidowicz-Bielak M et al. Efficacy and safety of a new surgical method to treat malignant glaucoma in pseudophakia. Eye (Lond) 2014; 28(6): 761-764. doi:10.1038/eye.2014.53.
5. Alza AG. Retroiridian anterior vitrectomy: a novel technique for the removal of late cortical remnants located in the posterior segment for anterior segment surgeons. Oftalmol Clin Exp 2024; 17(1): e128-e133. doi:10.70313/2718.7446.v17.n01.298