CLINICAL CASES
Macular serous detachment associated with optic disc pit: alternative treatment with pneumatic retinopexy and deferred laser
David Vladimir Diamint and Carla Pagano Boza
Hospital Italiano de Buenos Aires, Buenos Aires, Argentina.
Received: November 26th, 2024.
Approved: January 7th, 2025.
Corresponsal author
David Vladimir Diamint, MD.
Hospital Italiano de Buenos Aires
Tte. Gral. Juan Domingo Perón 4190
(C1199ABB) Buenos Aires
david.diamint@hospitalitaliano.org.ar
Conflicts of interest
The authors declare no conflict of interest.
Oftalmol Clin Exp (ISSNe 1851-2658)
2025; 18(1): e79-e84.
https://doi.org/10.70313/2718.7446.v18.n1.395
Abstract
Purpose: To describe a case of macular serous detachment associated with an optic disc pit successfully treated with pneumatic retinopexy and deferred laser photocoagulation.
Methods: We report the case of a patient with Down syndrome and macular serous detachment secondary to an optic disc pit. Pneumatic retinopexy with C3F8 gas was performed, followed by laser photocoagulation at the edge of the optic disc one week later. Visual acuity and macular thickness were assessed by optical coherence tomography during follow-up.
Results: The patient experienced a significant improvement in visual acuity and a reduction in macular detachment 2 months after the intervention. These results remained stable during the 3 years of follow-up. No complications associated with the treatment were observed.
Conclusion: Pneumatic retinopexy with deferred laser photocoagulation may be an effective and safe alternative in the treatment of macular serous detachment associated with an optic disc pit, especially in patients with contraindications or limitations for more invasive surgeries.
Keywords: Optic disc pit, macular serous detachment, pneumatic retinopexy, laser photocoagulation, Down syndrome.
Desprendimiento seroso sacular asociado a foseta papilar: tratamiento alternativo mediante retinopexia neumática y láser diferido
Resumen
Propósito: Describir un caso de desprendimiento seroso macular asociado a foseta papilar tratado exitosamente con retinopexia neumática y fotocoagulación láser diferida.
Métodos: Se presenta el caso clínico de una paciente con síndrome de Down y desprendimiento seroso macular secundario a foseta papilar. Se realizó una retinopexia neumática con gas C3F8 seguida de fotocoagulación láser en el borde del disco óptico una semana después. Se evaluó la agudeza visual y el grosor macular mediante tomografía de coherencia óptica durante el seguimiento.
Resultados: La paciente experimentó una mejoría significativa de la agudeza visual y una reducción del desprendimiento macular a los 2 meses de la intervención. Estos resultados se mantuvieron estables durante los 3 años de seguimiento. No se observaron complicaciones asociadas al tratamiento.
Conclusión: La retinopexia neumática con fotocoagulación láser diferida puede ser una alternativa eficaz y segura en el tratamiento del desprendimiento seroso macular asociado a foseta papilar, especialmente en pacientes con contraindicaciones o limitaciones para cirugías más invasivas.
Palabras clave: Foseta papilar, desprendimiento seroso macular, retinopexia neumática, fotocoagulación láser, síndrome de Down.
Desprendimiento seroso sacular asociado a foseta papilar: tratamiento alternativo mediante retinopexia neumática y láser diferido
Resumen
Propósito: Describir un caso de desprendimiento seroso macular asociado a foseta papilar tratado exitosamente con retinopexia neumática y fotocoagulación láser diferida.
Métodos: Se presenta el caso clínico de una paciente con síndrome de Down y desprendimiento seroso macular secundario a foseta papilar. Se realizó una retinopexia neumática con gas C3F8 seguida de fotocoagulación láser en el borde del disco óptico una semana después. Se evaluó la agudeza visual y el grosor macular mediante tomografía de coherencia óptica durante el seguimiento.
Resultados: La paciente experimentó una mejoría significativa de la agudeza visual y una reducción del desprendimiento macular a los 2 meses de la intervención. Estos resultados se mantuvieron estables durante los 3 años de seguimiento. No se observaron complicaciones asociadas al tratamiento.
Conclusión: La retinopexia neumática con fotocoagulación láser diferida puede ser una alternativa eficaz y segura en el tratamiento del desprendimiento seroso macular asociado a foseta papilar, especialmente en pacientes con contraindicaciones o limitaciones para cirugías más invasivas.
Palabras clave: Foseta papilar, desprendimiento seroso macular, retinopexia neumática, fotocoagulación láser, síndrome de Down.
Descolamento sacular seroso associado à fosseta papilar: tratamento alternativo com retinopexia pneumática e laser tardio
Resumo
Objetivo: Descrever um caso de descolamento seroso macular associado à fosseta papilar tratado com sucesso com retinopexia pneumática e fotocoagulação a laser tardia.
Métodos: Apresentamos o caso clínico de um paciente com síndrome de Down e descolamento seroso macular secundário a uma fosseta papilar. Foi realizada retinopexia pneumática com gás C3F8 seguida de fotocoagulação a laser na borda do disco óptico, uma semana depois. A acuidade visual e a espessura macular foram avaliadas por tomografia de coerência óptica durante o acompanhamento.
Resultados: O paciente apresentou melhora significativa na acuidade visual e redução do descolamento macular 2 meses após a cirurgia. Esses resultados permaneceram estáveis durante os 3 anos de acompanhamento. Não foram observadas complicações associadas ao tratamento.
Conclusão: A retinopexia pneumática com fotocoagulação a laser tardia pode ser uma alternativa eficaz e segura no tratamento do descolamento seroso macular associado à fosseta papilar, especialmente em pacientes com contraindicações ou limitações para cirurgias mais invasivas.
Palavras-chave: Fossa papilar, descolamento seroso macular, retinopexia pneumática, fotocoagulação a laser, síndrome de Down.
Introduction
Optic disc pit (ODP) is an uncommon congenital anomaly that consists of a defect in the lamina cribrosa of the optic nerve. It occurs equally in men and women, with an estimated incidence of 1 in 11,000 people1. It is usually unilateral and sporadic2, but can be bilateral in up to 15% of patients1. It can be asymptomatic or cause decreased visual acuity associated with serous macular detachment. Maculopathy associated with ODP develops in about 25%-75% of patients, between the second and fourth decades of life3-4.
The exact pathogenesis of serous detachment associated with ODP is unknown. Different hypotheses about the origin of subretinal fluid include: liquefied vitreous, cerebrospinal fluid, leaky blood vessels at the base of the ODP, or from the choroid1, 5-6.
If left to follow its natural course, this pathology has an unfavorable evolution in more than 75% of patients, with complications such as macular hole, foveolar cystic changes and degenerative changes of the retinal pigment epithelium. However, spontaneous resolution with visual improvement has been reported in 25% of cases4, 7.
In this article we present a case of maculopathy associated with ODP treated with pneumatic retinopexy and deferred laser, a minimally invasive treatment option that can be considered when, for different reasons, a more aggressive intervention is rejected or cannot be performed.
Case report
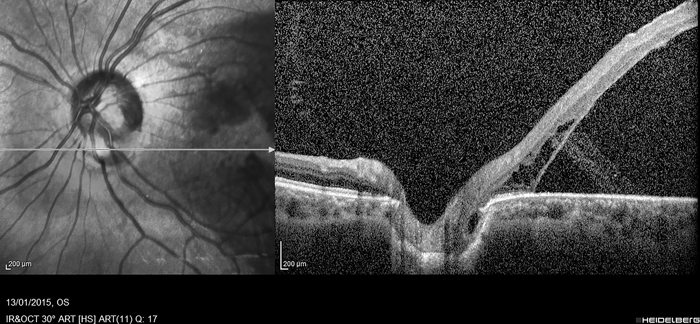
A 38-year-old caucasian woman with Down syndrome was referred for decreased visual acuity in the left eye. Her best-corrected visual acuity (BCVA) was 20/25 in the right eye and “count fingers” in the left eye. The pupils were symmetrical, round, reactive to light, with no relative afferent pupillary defect. Slit-lamp biomicroscopy revealed no anterior segment abnormalities. Intraocular pressure (IOP) was 14 mmHg in both eyes. Dilated fundus examination revealed a normal right eye and a defect in the temporal portion of the optic disc in the left eye, compatible with an optic disc pit (ODP), associated with a serous macular detachment. The peripheral retina was normal and attached. Spectral-domain optical coherence tomography (SD-OCT) (Fig. 1) and fluorescein angiography (FA) (Fig. 2) were performed to confirm the clinical findings. Her family refused vitrectomy, due to the need to perform the procedure under general anesthesia because of the Down syndrome, but accepted the possibility of a minimally invasive intervention that could be performed in the office. Therefore, pneumatic retinopexy was performed by injecting 0.3 ml of pure C3F8 into the vitreous cavity 4 mm from the corneal limbus with topical anesthesia. Anterior chamber paracentesis was performed to compensate for intraocular pressure. Face-down positioning was indicated for 1 week and then mild to moderate burns of 532 nm slit-lamp laser photocoagulation were performed on the superior, temporal and inferior border of the optic disc (Fig. 3). The patient was then instructed to continue face-down positioning for 2 more weeks.
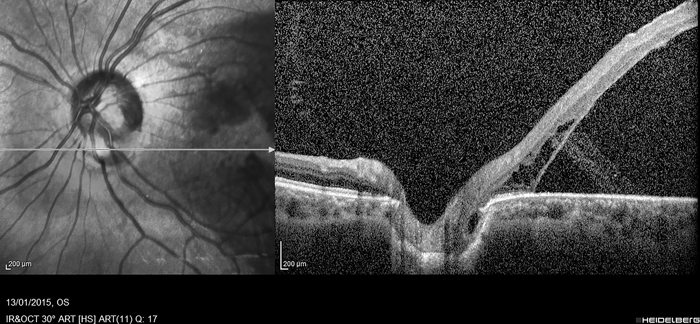
Figure 1. SD-OCT prior to treatment showing serous macular detachment.

Figure 2. Early and late phase fluorescein angiography showing leakage through the optic disc pit into the submacular space.
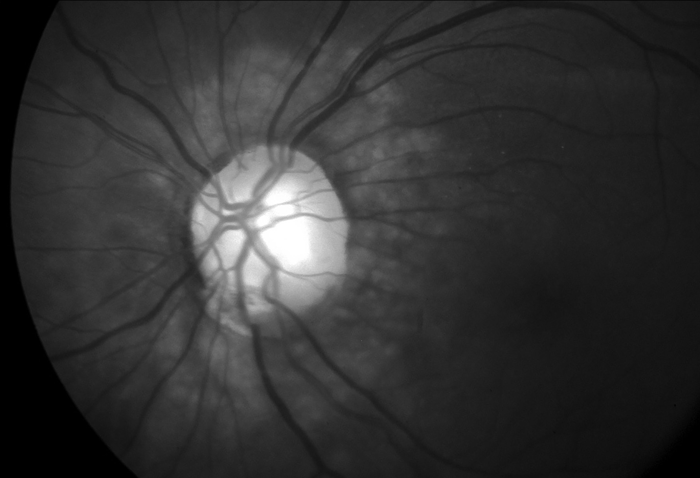
Figure 3. Mild to moderate laser burns at the superior, temporal, and inferior margins of the optic disc.
Close monthly follow-up was performed during the first year and every 3 months during the second and third years. SD-OCT was performed at each follow-up and FA was repeated at 12 months postoperatively. At 2 months after the intervention, BCVA improved from “count fingers” at 10 cm to 20/100. SD-OCT findings, which before the intervention showed a large serous macular detachment with a mean thickness of more than 800 µm, improved to a mean thickness of 389 µm at 2 months after surgery (Fig. 4). BCVA and macular thickness remained stable during the 3 years of follow-up. There were no complications associated with the treatment throughout follow-up.
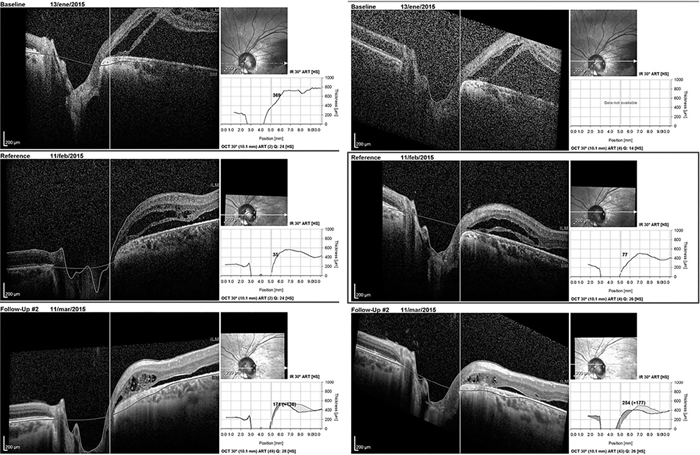
Figure 4. Comparative SD-OCT showing the progression of the macula before treatment (top), 1 month (center), and 2 months after the intervention (bottom).
Discussion
The diagnosis of optic disc pit (ODP) is made through dilated fundus examination. Fluorescein angiography confirms the diagnosis, as it shows the leakage of fluid from the ODP as the main source. SD-OCT helps to differentiate this pathology from others with macular detachment, since the typical macular retinoschisis is observed4. SD-OCT also helps to assess the severity and progression of serous detachment by reporting macular thickness.
There are a number of treatment options for this entity, which have been reported with varying success rates: laser photocoagulation alone, pneumatic retinopexy alone, macular buckling, pars plana vitrectomy with or without internal limiting membrane (ILM) peeling, tamponade with C3F8 or silicone oil, or a combination of the above8-9. Laser photocoagulation alone at the temporal margin of the disc is rarely possible in serous detachments due to ODP because of the separation of the neuroretina. A possible side effect, if the laser impacts are very intense and damage the nerve fiber layer, are paracentral scotomas10. Pneumatic retinopexy alone reduces subretinal fluid, but with a high recurrence rate since fluid leakage persists3. Pars plana vitrectomy with or without endolaser photocoagulation, ILM peeling and gas tamponade have been used successfully4, 9, 11-12. When mild to moderate laser is associated with any of the different possible procedures in this pathology, the success rate is increased without reporting severe side effects4. None of these treatments has been generally accepted, as there is not enough evidence to show that one is superior to the others.
The association of pneumatic retinopexy with face-down positioning and deferred laser photocoagulation has shown excellent long-term results3, and this clinical case is important, as it confirms the results published in previous research, a necessary condition in the scientific method. This treatment can be a good minimally invasive procedure with promising results both anatomically and physiologically. The rationale for this treatment is that the gas injected into the eye, combined with face-down rest, helps to displace the subretinal fluid, achieving the benefit that the laser is more effective, with less power, and, therefore, side effects are minimized.
Conclusion
Whatever the source of fluid in the macular serous detachment associated with the optic disc pit (ODP), creating a permanent barrier between the ODP and the macula helps to achieve resolution of the macular detachment. Pneumatic retinopexy with deferred laser photocoagulation contributes to the generation of a firm adhesion between the retinal pigment epithelium and the neuroretina, and is a good, minimally invasive and effective alternative to treat macular serous detachment associated with ODP, compared to vitreoretinal surgery.
References
1. Moisseiev E, Moisseiev J, Loewenstein A. Optic disc pit maculopathy: when and how to treat?: a review of the pathogenesis and treatment options. Int J Retin Vitr. 2015; 1(1): 13. doi:10.1186/s40942-015-0013-8
2. Martín-Begué N, Saint-Gerons M. Anomalías congénitas y del desarrollo del nervio óptico. Arch Soc Esp Oftalmol. 2016; 91(12): 577-588. doi:10.1016/j.oftal.2016.05.010
3. Lei L, Li T, Ding X et al. Gas tamponade combined with laser photocoagulation therapy for congenital optic disc pit maculopathy. Eye (Lond). 2015; 29(1): 106-114. doi:10.1038/eye.2014.245
4. Avci R, Yilmaz S, Inan UU, et al. Long-term outcomes of pars plana vitrectomy without internal limiting membrane peeling for optic disc pit maculopathy. Eye (Lond). 2013; 27(12): 1359-1367. doi:10.1038/eye.2013.172
5. Gass JD. Serous detachment of the macula: secondary to congenital pit of the optic nervehead. Am J Ophthalmol. 1969; 67(6): 821-841.
6. Regenbogen L, Stein R, Lazar M. Macular and juxtapapillar serous retinal detachment associated with pit of optic disc. Ophthalmologica. 1964; 148: 247-251.
7. Cruzado-Sánchez D, Valdivieso HL, Nájar SML. Resolución espontánea del desprendimiento macular asociado a anomalías congénitas del nervio óptico: coloboma del disco óptico y foseta papilar. Arch Soc Esp Oftalmol. 2013; 88(5): 201-203. doi:10.1016/j.oftal.2012.09.030
8. Sanghi G, Padhi TR, Warkad VU et al. Optical coherence tomography findings and retinal changes after vitrectomy for optic disc pit maculopathy. Indian J Ophthalmol. 2014; 62(3): 287-290. doi:10.4103/0301-4738.111191
9. Mohammed OA, Pai A. Inverted autologous internal limiting membrane for management of optic disc pit with macular detachment. Middle East Afr J Ophthalmol. 2013; 20(4): 357-359. doi:10.4103/0974-9233.120008
10. Diab F, Al-Sabah K, Al-Mujaini A. Successful surgical management of optic disc pit maculopathy without internal membrane peeling. Middle East Afr J Ophthalmol. 2010; 17(3): 278-280. doi:10.4103/0974-9233.65495
11. Hirakata A, Inoue M, Hiraoka T, McCuen BW. Vitrectomy without laser treatment or gas tamponade for macular detachment associated with an optic disc pit. Ophthalmology. 2012; 119(4): 810-818. doi:10.1016/j.ophtha.2011.09.026
12. Bakri SJ, Beer PM. Vitreoretinal surgery for optic pit associated serous macular detachment: a discussion of two cases. Int Ophthalmol. 2004; 25(3): 143-146. doi:10.1007/s10792-004-5197-0