ORIGINAL ARTICLES
Presbyopia and age-related macular degeneration: a survey on spectacle lens design
Abel Szepsa-b, Juan Manuel Suarezc, Valeria Bordesed, Matías Acerbie, Roberto Albertazzif, Mario Saraviag, Guillermo Iribarrenh, José Luna Pintoi, Carla Lancaj-k, Rafael Iribarreng-h
aHospital Posadas, Buenos Aires, Argentina
b+ Ophthalmology, Buenos Aires, Argentina.
cSuarez Optical Lab, Buenos Aires, Argentina.
dValeria Bordese Espacio Óptico, Córdoba, Argentina.
eFoucault Optical Center, Buenos Aires, Argentina.
fQuilmes Ophthalmological Center, Quilmes, Argentina.
gRetina Foundation, Buenos Aires, Argentina.
hDrs. Iribarren Eye Consultants, Buenos Aires, Argentina.
iVer Foundation, Buenos Aires, Argentina.
jEscola Superior de Tecnologia da Saúde de Lisboa (ESTeSL), Instituto Politécnico de Lisboa, Lisboa, Portugal.
kComprehensive Health Research Center (CHRC), Escola Nacional de Saúde Pública, Universidade Nova de Lisboa, Lisboa, Portugal,
Received: August 7th, 2024.
Approved: November 12nd, 2024.
Corresponsal author
Dr. Abel Szeps
Gavilán 4103
(C1419ENM) Buenos Aires
abelszeps@gmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2024; 17(4): e571-e578.
https://doi.org/10.70313/2718.7446.v17.n04.368
Conflict of interest
Abel Szeps and Rafael Iribarren work for NOVAR, the manufacturer of the peripheral hyperopic defocus special spectacle. Other authors declare no conflict of interest.
Abstract
Objective: To evaluate the design of spectacle lenses and daily spectacle use in presbyopes over 60 years of age with and without age-related macular degeneration (AMD).
Methods: A cross sectional study was designed, and a web questionnaire was distributed to a two ophthalmological centers database of presbyopic outpatients over 60 years of age with and without AMD. The questionnaire included data of monofocal, bifocal or multifocal spectacle use, and asked whether the subjects used their spectacles full day or only for reading purposes. A multivariate logistic regression analysis was performed to test whether full or part day spectacle use, and use of multifocals or bifocals were associated with the odds of AMD, controlling by age, gender and cataract surgery.
Results: The sample included 780 subjects, of which 379 (48.6%) had AMD; 61.3% were women. Glasses were used only for near vision by 60.9% of the individuals, while 26.0% used either bifocals or multifocals as full time wearers. Increasing age (odds ratio [OR]: 1.04, 95% CI 1.02 to 1.06, p<0.001), undergoing cataract surgery (OR: 3.10, 95%CI 2.07 to 4.65, p<0.001) and wearing glasses all day (OR: 1.94, 95%CI 1.29 to 2.91, p=0.001) were associated with the presence of AMD.
Conclusions: We found an association between the presence of AMD and full-time spectacle wear. Further prospective controlled studies are necessary to study the link between spectacle use and AMD development.
Keywords: presbyopia, AMD, multifocal glasses, bifocal glasses, monofocal glasses.
Presbicia y degeneración macular asociada a la edad: una encuesta sobre el diseño de las lentes oftálmicas
Resumen
Objetivo: Evaluar el diseño de las lentes oftálmicas y el uso diario de anteojos en présbitas mayores de 60 años con y sin degeneración macular asociada a la edad (DMAE).
Métodos: Se diseñó un estudio transversal y se distribuyó un cuestionario web a una base de datos de dos centros oftalmológicos de pacientes externos présbitas mayores de 60 años con y sin DMAE. El cuestionario incluía datos de uso de anteojos monofocales, bifocales o multifocales, y preguntaba acerca de si los sujetos usaban los anteojos todo el día o sólo para leer. Se realizó un análisis de regresión logística multivariada para comprobar si el uso de anteojos durante todo el día o parte de él y el uso de gafas multifocales o bifocales se asociaba con la probabilidad de padecer DMAE, teniendo en cuenta la edad, el sexo y la cirugía de cataratas.
Resultados: La muestra incluyó 780 sujetos, de los cuales 379 (48,6%) tenían DMAE; el 61,3% eran mujeres. El 60,9% de los individuos utilizaba anteojos sólo para ver de cerca, mientras que el 26,0% utilizaba bifocales o multifocales a tiempo completo. El aumento de la edad (odds ratio [OR]: 1,04; IC 95%: 1,02 a 1,06; p<0,001), la cirugía de cataratas (OR: 3,10; IC 95%: 2,07 a 4,65; p<0,001) y el uso de gafas durante todo el día (OR: 1,94; IC 95%: 1,29 a 2,91; p=0,001) se asociaron con la presencia de DMAE.
Conclusiones: Encontramos una asociación entre la presencia de DMAE y el uso de anteojos a tiempo completo. Son necesarios más estudios prospectivos controlados para estudiar la relación entre el uso de anteojos y el desarrollo de DMAE.
Palabras clave: presbicia, DMAE, lentes multifocales, lentes bifocales.
Presbiopia e degeneração macular relacionada à idade: uma pesquisa sobre design de lentes oftálmicas
Resumo
Objetivo: Avaliar o design de lentes oftálmicas e o uso diário de óculos em presbitas acima de 60 anos com e sem degeneração macular relacionada à idade (DMRI).
Métodos: Foi desenhado um estudo transversal e um questionário web foi distribuído a uma base de dados de dois centros oftalmológicos de pacientes ambulatoriais presbiópicos com mais de 60 anos de idade com e sem DMRI. O questionário incluiu dados sobre o uso de óculos monofocais, bifocais ou multifocais e perguntou se os sujeitos usavam óculos o dia todo ou apenas para leitura. Foi realizada análise de regressão logística multivariada para verificar se o uso de óculos durante todo ou parte do dia e o uso de óculos multifocais ou bifocais estavam associados à probabilidade de sofrer de DMRI, levando em consideração idade, sexo e idade de cirurgia de catarata.
Resultados: A amostra incluiu 780 indivíduos, dos quais 379 (48,6%) apresentavam DMRI; 61,3% eram mulheres. 60,9% dos indivíduos usavam óculos apenas para visão de perto, enquanto 26,0% usavam óculos bifocais ou multifocais em tempo integral. Aumento da idade (odds ratio [OR]: 1,04; IC 95%: 1,02 a 1,06; p<0,001), cirurgia de catarata (OR: 3,10; IC 95%: 2,07 a 4,65; p<0,001) e uso de óculos ao longo do dia (OR: 1,94; IC 95%: 1,29 a 2,91; p=0,001) estiveram associados à presença de DMRI.
Conclusões: Encontramos associação entre a presença de DMRI e o uso de óculos em tempo integral. Mais estudos prospectivos controlados são necessários para estudar a relação entre o uso de óculos e o desenvolvimento da DMRI.
Palavras-chave: presbiopia, DMRI, lentes multifocais, lentes bifocais.
Introduction
Many risk factors related to age related macular degeneration (AMD) have been described. Older age, gender, genetic background, and certain lifestyle habits such as smoking history, ultraviolet light exposure, sedentarism, metabolic syndrome, hypertension, and low vegetable intake have been associated with the development of AMD1-5. Myopic refractive error is known to be protective for AMD and some cross sectional studies have found that more hyperopic refractions are positively correlated with higher odds of developing AMD6-11.
Some aspects of the relationship between AMD and hyperopic correction remain not well studied. Unresolved issues rise questions related with the possible mechanisms at play, such as if the risk is related with the hyperopic correction, the amount of daily spectacle use or the design of the glasses (multifocals vs. monofocals). Positive lenses like the ones used in presbyopic years, have been recently shown to increase choroidal thickness by a significant amount12-13. Our group has shown recently that this increase is more pronounced in AMD subjects, raising the question of whether choroidal thickness modulation by spectacle use could be a risk factor in AMD development13. Following this line of ideas, the aim of the present study was to find the possible association between the design and type of spectacle lenses and the amount of time they are worn in daily life by presbyopes 60 years old with or without AMD.
Material and methods
A web questionnaire was developed asking for spectacle type and use in two unselected samples of adult subjects. The questionnaire was distributed both among normal subjects on one hand and subjects with AMD on the other. As no intervention was performed (except gathering data anonymously) the ethics committee of the Argentinian Council of Ophthalmology, who was consulted, waived approval for the study. The questionnaire included data of age and gender, past cataract or refractive surgery, usual monofocal, bifocal or multifocal spectacle use, and subjects were also asked whether they used their spectacles full day or only for reading purposes. This last question attempted to distinguish full-time users (probably hyperopic presbyopes with higher prescriptions) from those who only use correction at near (probably emmetropic or low hyperopic presbyopes). Myopic subjects were not included in this study (the invitation to participate in the study mentioned that myopes should not answer the questionnaire).
During the period between November 2023 and March 2024 the questionnaire was distributed among three low vision services attending AMD subjects. These were Bordese, Foucault and Suarez low vision optical stores, where consecutive AMD subjects were surveyed during the mentioned period. The questionnaire was also distributed simultaneously by email to a database of 35,000 outpatients who regularly attended scheduled ophthalmological clinical check-ups in two ophthalmology centers (Drs. Iribarren Eye Consultants and Quilmes Ophthalmology Center). In this case, adult subjects aged 60+ without AMD were asked to answer the questionnaire and served as controls. For AMD subjects, the separate questionnaire also inquired about how many years they had been diagnosed with the disease and asked about the treatment they were currently receiving.
Statistical analysis
The results of age as a numerical variable are expressed as mean and standard deviation. Nominal variables like gender or spectacle use are expressed as absolute frequency and percentage. A multivariate logistic regression analysis was performed to test whether full or part day spectacle use, and use of multifocals or bifocals were associated with the odds of AMD, controlling for age, gender and cataract surgery. A p-value ≤ 0.05 was taken as significant. Excel tables (Microsoft, USA) and SPSS 25 statistical software (IBM, USA) were used for the analysis.
Results
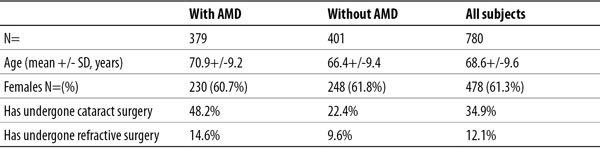
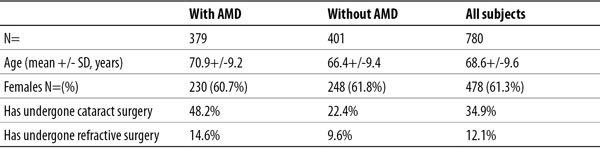
Descriptive statistics of both groups are presented in Table 1. The sample consisted of 780 subjects of which 379 had AMD (48.6%). There were 478 females (61.3%) and there were no significant differences in the distribution of gender by groups of AMD or control subjects. In all, 34.4% of subjects had undergone cataract surgery and 12.1% had undergone some type of refractive surgery to avoid using spectacles. AMD subjects reported higher frequency of cataract surgery than controls (48.2% vs. 22.4%, p<0.001) and were in average 5 years older than the controls (p<0.01). Among subjects with AMD, 129 (34.0%) were receiving antiangiogenic treatment, 110 (29.0%) were under vitamins and 35 (9.3%) used low vision aids. On average, the time since diagnosis up to the time of the interview in the low vision service was one year for those with any type of AMD.
Table 1. Descriptive statistics of both groups.
Regarding spectacle type, 60.9% of the individuals in the whole sample reported using glasses only for near purposes, while 26.0% used either bifocals or multifocals (and the rest reported no spectacle use). When the question asked whether the spectacles were used only for near or full time, 59.9% reported using spectacles only for near compared to 40.1% of full time wearers.
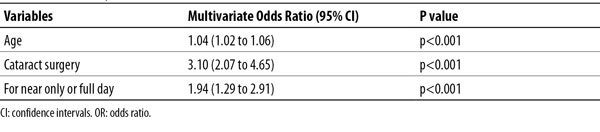
A logistic regression model was performed to ascertain the effects of age, gender, cataract surgery, refractive surgery, and type or time of spectacle use, on the presence of AMD. The model explained 19.7% (Nagelkerke R2) of the variance in AMD and correctly classified 68.1% of cases. Increasing age (Odds ratio [OR]: 1.04, 95% Confidence Intervals [CI] 1.02 to 1.06, p<0.001), having cataract surgery (OR:3.10, 95% 2.07 to 4.65, p<0.001) and using lenses full day (OR:1.94, 95% 1.29 to 2.91, p=0.001) were associated with the presence of AMD. As was expected, the use of multifocal or bifocal glasses compared to monofocal lenses was negatively associated with macular degeneration, but this was significant only in univariate analysis (p<0.001, Table 2).
The model was adjusted for gender, refractive surgery, and type of glasses.
Table 2. Association of key risk factors alone and in combination with AMD.
Discussion
The relationship between refractive error and AMD has been shown to be controversial to some extent14. To our knowledge, the study of the time and type of spectacle use in presbyopic individuals as possible risk factors for AMD has not been previously explored. The idea for this study was developed by our group while working in myopia control methods. It was known from the literature that positive lenses applied to animals and humans increased choroidal thickness within minutes, whereas negative lenses decreased choroidal thickness12. It was also well known that longer myopic eyes had 50 microns thinner choroids, and that shorter hyperopic eyes had choroids 50 microns thicker than those of their emmetropic peers15-16. But the reason for these differences has only been discussed in terms of longer eyes having thinner choroids by a mechanical explanation15. Choroidal thickness is classically understood as an adaptation of the vascular tissue to longer or shorter eyes, with well-determined circadian rhythms of changing thickness17. Recently, it was discovered that negative lenses in human subjects make the choroid thinner in few minutes as was known from animal studies18, while positive lenses make the choroid thicker12, through a respective decrease or increase in choroidal blood flow19.
In novel experiments we demonstrated that the choroid of adult subjects increased thickness when reading with usual spectacles for 20 minutes by 25 microns, and that this increase was more pronounced in AMD subjects20. In these last experiments it was also shown that, with a special peripheral hyperopic defocus lens design, the choroidal thickening produced by reading with usual spectacles could be reversed in another 20 minutes of reading with the special defocus spectacles. This fact suggests that thicker choroids in hyperopes could be in part due to the common use of positive spectacles by humans, while the common use of negative lenses in myopes would produce thinner choroids.
The mechanism driving these changes is the retinal decoding of defocus21, a mechanism probably based on chromatic aberration detection which in turn sends a signal for STOP or GROW in the developing eye18. This retinal signalling involves dopamine amacrine cells, nitric oxide in the inner retina, and the modulation of the synthesis of retinoic acid in the pigmentary epithelium or interleukin-6 in the choroid22-24. It has been known that defocus governs choroidal thickness and eye growth from experiments done in animals and humans for more than 40 years by now25.
On the other hand, the pathophysiology of AMD comprises choroidal thickness and its blood flow involving several molecules related to inflammation and apoptosis2-4, 26. In recent years pachychoroidal diseases27 are thought as complex interplay in which a thicker choroid with increased blood flow may compress the coriocapilaris with less perfusion, hypoxia and less turnover of deposited lipofucsin at Bruck’s membrane28-29. In this sense molecules like retinoic acid and interleukine-6 could increase the inflammatory process and pigmentary cells apoptosis at this level30.
In our defocus and AMD study, the recovery of choroidal thickness with the peripheral hyperopic defocus device was smaller in AMD cases20, which would indicate that choroidal dysfunction and choroidal thickening demanded by conventional lenses in presbyopia could be a non-explored risk factor in AMD. In the present cross-sectional study, surveyed data show increased odds ratio for the presence of AMD in full-time spectacle wearers in the multivariate controlled analysis, and a negative correlation for users of multifocals or bifocals for AMD when compared to monofocals (univariate analysis). This could be in line with some protective effect of certain multifocal or bifocal glasses on the development of AMD in presbyopic subjects. Nevertheless, some questions remain unanswered. Would monofocal use of near-glasses by the phakic or pseudophakic presbyopic patient be a non-explored risk factor for the development of maculopathy? Would the choice of multifocal or EDOF IOLs for cataract surgery affect the possible prevention of future AMD? Research in this area is in need before glasses with choroidal control technology (with Hyperopic Peripheral Defocus) are prescribed for presbyopic subjects.
There are several limitations of the current study. Validity and reliability of the questionnaire were not tested. Furthermore, the study had a cross-sectional design, and further well-designed studies are necessary to confirm or deny these findings. Other authors have proposed that the lower prevalence of AMD in myopic subjects could be due to lower light intensity reaching the retina in longer myopic eyes31. It is interesting to note that illumination is also crucial in the modulation of choroidal thickness32. So much could be explored in this sense. Another important limitation in this study is that family history of AMD and smoking for example, two known risk factors for AMD, were not explored in the survey. Future studies could explore these and other known risk factors for AMD to include them in the statistical models and find out to what extent this possible new factor of reading with plus lenses stays significant.
Conclusion
This study shows an association between continuous positive spectacle use for presbyopia and presence of AMD. To find a possible causal relationship in this sense, the incidence of new cases of AMD should be explored on a population basis in datasets that may include refractive error data. Spectacle use could also be explored with questionnaires like the present one, or even with actual refractive error assessment in systematic studies.
References
1. Choudhury F, Varma R, McKean-Cowdin R, Klein R, Azen SP; Los Angeles Latino Eye Study Group. Risk factors for four-year incidence and progression of age-related macular degeneration: the Los Angeles Latino Eye Study. Am J Ophthalmol 2011; 152(3): 385-395. doi:10.1016/j.ajo.2011.02.025.
2. Bowes Rickman C, Farsiu S, Toth CA, Klingeborn M. Dry age-related macular degeneration: mechanisms, therapeutic targets, and imaging. Invest Ophthalmol Vis Sci 2013; 54(14): ORSF68-ORSF80. Published 2013 Dec 13. doi:10.1167/iovs.13-12757.
3. Vyawahare H, Shinde P. Age-related macular degeneration: epidemiology, pathophysiology, diagnosis, and treatment. Cureus 2022; 14(9): e29583. Published 2022 Sep 26. doi:10.7759/cureus.29583.
4. Seddon JM. Macular degeneration epidemiology: nature-nurture, lifestyle factors, genetic risk, and gene-environment interactions: the Weisenfeld Award Lecture. Invest Ophthalmol Vis Sci 2017; 58(14): 6513-6528. doi:10.1167/iovs.17-23544.
5. Jonas JB, Nangia V, Kulkarni M, Gupta R, Khare A. Associations of early age-related macular degeneration with ocular and general parameters. The Central India Eyes and Medical Study. Acta Ophthalmol 2012; 90(3): e185-e191. doi:10.1111/j.1755-3768.2011.02316.x.
6. Li Y, Wang J, Zhong X, et al. Refractive error and risk of early or late age-related macular degeneration: a systematic review and meta-analysis. PLoS One 2014; 9(3): e90897. Published 2014 Mar 6. doi:10.1371/journal.pone.0090897.
7. Hashimoto S, Yasuda M, Fujiwara K, et al. Association between axial length and myopic maculopathy: The Hisayama Study [published correction appears in Ophthalmol Retina. 2022 Mar;6(3): 258-259. doi:10.1016/j.oret.2020.09.009]. Ophthalmol Retina 2019; 3(10): 867-873. doi:10.1016/j.oret.2019.04.023.
8. Sato M, Minami S, Nagai N, et al. Association between axial length and choroidal thickness in early age-related macular degeneration. PLoS One 2020; 15(10): e0240357. Published 2020 Oct 9. doi:10.1371/journal.pone.0240357.
9. Ikram MK, van Leeuwen R, Vingerling JR, Hofman A, de Jong PT. Relationship between refraction and prevalent as well as incident age-related maculopathy: the Rotterdam Study. Invest Ophthalmol Vis Sci 2003; 44(9): 3778-3782. doi:10.1167/iovs.03-0120.
10. Lavanya R, Kawasaki R, Tay WT, et al. Hyperopic refractive error and shorter axial length are associated with age-related macular degeneration: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci 2010; 51(12): 6247-6252. doi:10.1167/iovs.10-5229.
11. Sandberg MA, Tolentino MJ, Miller S, Berson EL, Gaudio AR. Hyperopia and neovascularization in age-related macular degeneration. Ophthalmology 1993; 100(7): 1009-1013. doi:10.1016/s0161-6420(93)31546-0.
12. Read SA, Collins MJ, Sander BP. Human optical axial length and defocus. Invest Ophthalmol Vis Sci 2010; 51(12): 6262-6269. doi:10.1167/iovs.10-5457.
13. Szeps A, Suarez JM, Torres R, Iribarren R. Choroidal control technology: new horizons in maculopathy and presbyopia. Graefes Arch Clin Exp Ophthalmol. Published online September 7, 2024. doi:10.1007/s00417-024-06633-4.
14. Pan CW, Ikram MK, Cheung CY, et al. Refractive errors and age-related macular degeneration: a systematic review and meta-analysis. Ophthalmology 2013; 120(10): 2058-2065. doi:10.1016/j.ophtha.2013.03.028.
15. Lee GY, Yu S, Kang HG, Kim JS, Lee KW, Lee JH. Choroidal thickness variation according to refractive error measured by spectral domain-optical coherence tomography in Korean children. Korean J Ophthalmol 2017; 31(2): 151-158. doi:10.3341/kjo.2017.31.2.151.
16. Kim M, Kim SS, Koh HJ, Lee SC. Choroidal thickness, age, and refractive error in healthy Korean subjects. Optom Vis Sci 2014; 91(5): 491-496. doi:10.1097/OPX.0000000000000229.
17. Nickla DL, Wallman J. The multifunctional choroid. Prog Retin Eye Res 2010; 29(2): 144-168. doi:10.1016/j.preteyeres.2009.12.002.
18. Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia [published correction appears in Neuron. 2012 Apr 12;74(1):207]. Neuron 2004; 43(4): 447-468. doi:10.1016/j.neuron.2004.08.008.
19. Swiatczak B, Schaeffel F, Calzetti G. Imposed positive defocus changes choroidal blood flow in young human subjects. Graefes Arch Clin Exp Ophthalmol 2023; 261(1): 115-125. doi:10.1007/s00417-022-05842-z.
20. Szeps A, Suarez JM, Torres R, Iribarren R. Choroidal control technology: new horizons in maculopathy and presbyopia. Graefes Arch Clin Exp Ophthalmol. Published online September 7, 2024. doi:10.1007/s00417-024-06633-4.
21. Swiatczak B, Schaeffel F. Myopia: why the retina stops inhibiting eye growth. Sci Rep 2022; 12(1): 21704. Published 2022 Dec 15. doi:10.1038/s41598-022-26323-7.
22. Troilo D, Smith EL 3rd, Nickla DL, et al. IMI: report on experimental models of emmetropization and myopia. Invest Ophthalmol Vis Sci 2019; 60(3): M31-M88. doi:10.1167/iovs.18-25967.
23. Stone RA. Myopia pharmacology: etiologic clues, therapeutic potential. In: Yorio T, Clark AF, Wax MB (eds.). Ocular therapeutics: eye on new discoveries. New York: Elsevier Academic, 2008, p. 167-196.
24. Summers JA, Martínez E. Visually induced changes in cytokine production in the chick choroid. Elife 2021; 10: e70608. doi:10.7554/eLife.70608.
25. Schaeffel F, Swiatczak B. Mechanisms of emmetropization and what might go wrong in myopia. Vision Res 2024; 220: 108402. doi:10.1016/j.visres.2024.108402.
26. Ambati J, Ambati BK, Yoo SH, Ianchulev S, Adamis AP. Age-related macular degeneration: etiology, pathogenesis, and therapeutic strategies. Surv Ophthalmol 2003; 48(3): 257-293. doi:10.1016/s0039-6257(03)00030-4.
27. Yanagi Y. Pachychoroid disease: a new perspective on exudative maculopathy. Jpn J Ophthalmol 2020; 64(4): 323-337. doi:10.1007/s10384-020-00740-5.
28. Daruich A, Matet A, Dirani A, et al. Central serous chorioretinopathy: recent findings and new physiopathology hypothesis. Prog Retin Eye Res 2015; 48: 82-118. doi:10.1016/j.preteyeres.2015.05.003.
29. Luo Z, Xu Y, Xu K, et al. Choroidal vortex vein drainage system in central serous chorioretinopathy using ultra-widefield optical coherence tomography angiography. Transl Vis Sci Technol 2023; 12(9): 17. doi:10.1167/tvst.12.9.17.
30. Noy N. Between death and survival: retinoic acid in regulation of apoptosis. Annu Rev Nutr 2010; 30: 201-217. doi:10.1146/annurev.nutr.28.061807.155509.
31. Quigley MG, Powell I, Wittich W. Increased axial length corresponds to decreased retinal light dose: a parsimonious explanation for decreasing AMD risk in myopia. Invest Ophthalmol Vis Sci 2018; 59(10): 3852-3857. doi:10.1167/iovs.17-23696.
32. Chakraborty R, Baranton K, Spiegel D, et al. Effects of mild- and moderate-intensity illumination on short-term axial length and choroidal thickness changes in young adults. Ophthalmic Physiol Opt 2022; 42(4): 762-772. doi:10.1111/opo.12988.