
ORIGINAL ARTICLES
Effect of vertex distance in the treatment area of myopia control spectacles
Martín de Tomása, Abel Szepsb, Gabriel Martína,c, Guillermo Saraccod, Carla Lancae, Rafael Iribarrena,f-g
aOpulens (Novar), Buenos Aires, Argentina.
bDeparment of Ophthalmology, Posadas Hospital, Buenos Aires. Argentina.
cReichert Technologies, Depew, New York, USA.
dSaracco Optical Center, Buenos Aires, Argentina.
eComprehensive Health Research Center (CHRC), Escola Nacional de Saúde Pública, Universidade Nova de Lisboa, Lisboa, Portugal.
fDrs. Iribarren Eye Consultants, Buenos Aires, Argentina.
gRetina Foundation, Buenos Aires, Argentina.
Received: August 27th, 2024.
Approved: October 15th, 2024
Corresponsal author
Rafael Iribarren, MD
Arenales 981
(1061) Buenos Aires, Argentina
+54-911-5147-9312
rafairibarren@gmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2024; 17(4): e547-e553.
https://doi.org/10.70313/2718.7446.v17.n04.367
Conflict of interest declaration
Abel Szeps, Martin de Tomas and Rafael Iribarren are consultants of NOVAR. Gabriel Martín works for NOVAR and Opulens.
Abstract
Purpose: To analyze the size of treatment area produced by possible myopia control spectacles at two different vertex distances.
Methods: An experimental study was designed. Two visual fields were performed in an Octopus 123 automatic perimeter (Interzeag, Germany), with an opaque frame of 37 mm diameter including a central hole of 8 mm wide, fitted in the trial lenses from the perimeter, with two different vertex distances (6 mm and 12 mm) in a 60 years-old subject. The frame around the central hole represents the treatment area of commercially available myopia control spectacles which have a central round zone for clear distance vision.
Results: The visual field with a 12 mm vertex distance showed an expected circular loss of sensitivity at approximately 12°. While the 6mm vertex distance visual field showed an almost normal visual field.
Conclusion: A normal vertex distance produces better area of treatment than a shorter one in myopia control spectacles. The results of the present study suggest that vertex distance should be rigorously monitored in myopia control practice and research.
Keywords: myopia control, spectacles, treatment area, visual fields.
Efecto de la distancia del vértice en la zona de tratamiento de las gafas de control de la miopía
Resumen
Objetivo: Analizar el tamaño del área de tratamiento producida por las posibles gafas de control de la miopía con dos distancias de vértice diferentes.
Materiales y métodos: Se diseñó un estudio experimental. Se realizaron dos campos visuales en un perímetro automático Octopus 123 (Interzeag, Alemania), con una montura opaca de 37 mm de diámetro que incluía un agujero central de 8 mm de ancho, colocado en las lentes de prueba desde el perímetro, con dos distancias de vértice diferentes (6 mm y 12 mm) en un sujeto de 60 años. La montura alrededor del agujero central representa la zona de tratamiento de las gafas de control de la miopía disponibles en el mercado, que tienen una zona central redonda para una visión clara de lejos.
Resultados: El campo visual con una distancia de vértice de 12 mm mostró una pérdida de sensibilidad circular esperada de aproximadamente 12°. Mientras que el campo visual con una distancia de vértice de 6 mm mostró un campo visual casi normal.
Conclusiones: Una distancia de vértice normal produce mejor área de tratamiento que una más corta en gafas de control de miopía. Los resultados del presente estudio sugieren que la distancia de vértice debería controlarse rigurosamente en la práctica y la investigación del control de la miopía.
Palabras clave: control de la miopía, gafas, área de tratamiento, campos visuales.
Efeito da distância do vértice na zona de tratamento dos óculos de controle de miopia
Resumo
Objetivo: Analisar o tamanho da área de tratamento produzida por possíveis óculos de controle de miopia com duas distâncias de vértice diferentes.
Materiais e métodos: Foi desenhado um estudo experimental. Dois campos de visão foram realizados em um perímetro automático Octopus 123 (Interzeag, Alemanha), com moldura opaca de 37 mm de diâmetro que incluía um orifício central de 8 mm de largura, colocado nas lentes de teste a partir do perímetro, com duas distâncias de vértices diferentes. (6 mm e 12 mm) em sujeito de 60 anos. A armação ao redor do orifício central representa a zona de tratamento dos óculos de controle de miopia disponíveis no mercado, que possuem uma zona central redonda para visão clara à distância.
Resultados: O campo visual com distância do vértice de 12 mm apresentou perda de sensibilidade circular esperada de aproximadamente 12°. Enquanto o campo visual com distância do vértice de 6 mm apresentou um campo visual quase normal.
Conclusões: Uma distância normal do vértice produz uma melhor área de tratamento do que uma distância mais curta em óculos de controle de miopia. Os resultados do presente estudo sugerem que a distância do vértice deve ser rigorosamente controlada na prática e pesquisa de controle da miopia.
Palavras-chave: controle da miopia, óculos, área de tratamento, campos visuais.
Introduction
During the last years basic and clinical researchers have developed myopia control spectacles based on peripheral myopic defocus or decreased contrast with central distance correction apertures ranging from 7mm to 15mm1-7. Recent studies suggest that the retina may detect the sign of defocus which controls ocular growth by computing the relative contrast sensitivity of S and L cones based on longitudinal chromatic aberration8-9. As S cones (blue frequency) are absent in the foveal zone, more research on the perifoveal macular areas that include the three types of cones (S, M and L) is important. Using multifocal electroretinogram, a previous study showed that the area around the 6° from de fovea is the most sensitive sector of the retina to detect defocus10. These findings align with previous experiments of Earl Smith in 2005 showing that foveal ablation with laser beams did not alter much the emmetropization mechanisms in the monkey model11-12. Additionally, peripheral defocus contact lenses13 and peripheral defocus spectacles14 have showed good results in controlling myopia progression in children.
In a previous study, we aimed to know which areas of the retina were out of focus in myopia control spectacles. Using posterior optical coherence tomography (OCT) images we showed for the first time the projection of retinal shadows from different defocus spectacles15. During our experiments we noticed that the amplitude of the in-focus and out-of-focus areas in the images depended on the vertex distance at which the glasses were fitted. We also noted that decreasing vertex distance enlarged the central clear zone at the retinal plane (and vice versa). To correctly quantify this effect, we developed a study to determine the corresponding changes in visual fields using a diaphragm at two different vertex distances. This study shows the results of those experiments and discusses our findings in the context of myopia control treatment.
Methods
An experimental study was designed. Two visual fields were prformeed, in an Octopus 123 automatic perimeter (Interzeag, Germany), with a round and opaque whiteboard frame fitted in a 37mm diameter lens probe. The frame included a central hole 8 mm wide and was fitted in the trial lenses slot of the perimeter, with two different vertex distances. Octopus 123 perimeter has two different vertex distances separated by 6mm (Figure 1). All vertex distances were measured with a ruler (Bernell, USA) fitting the subject in place with the opaque frame and taking photographs from the side at 90° angles. The ruler was included in the photograph, such that with computer software and calipers the photos could be studied comparing the vertex distances with the actual millimeters in the ruler (Figs. 1 & 2). Two different vertex distances were used to perform the visual fields (6 mm and 12 mm) considering that the perimeter has two slots for the trial lenses. The visual fields were performed in one voluntary subject of female sex with 60 years-old, with no ocular pathology, and 20/20 uncorrected distance visual acuity with known normal visual fields. This study was conducted in accordance with the tenets of the Declaration of Helsinki. The Ethics Committee of the Argentinian Council of Ophthalmology stated that no ethics approval was needed for this study that did not include patients or any intervention.

Figure 1. Locations of the two slots for the trial lenses in the Octopus 123 perimeter, with a ruler showing 6 mm distance between them.
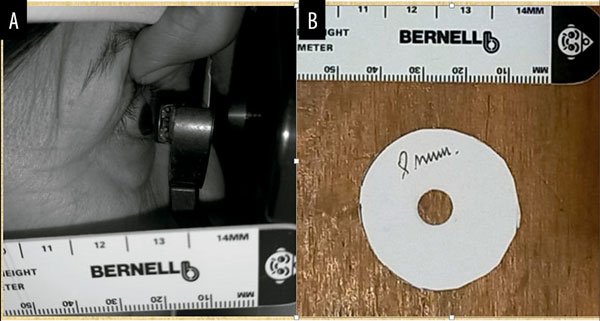
Figure 2. A) Subject’s 12mm vertex distance with the opaque frame with an 8 mm hole located in the farthest slot of the perimeter. B). Round whiteboard opaque frame with an 8 mm hole.
The visual fields (white-on-white automated perimetry) were performed as usual in a darkened room and central fixation was constantly checked in the computer display of the perimeter. Pupil diameter was 4.5 mm during the testing in both visual fields. The testing included the 60° of the central visual field of the right eye and the TOP program of the machine was used with a cross for central fixation. Both visual fields were tested in the same eye on different days after 10 minutes of adaptation to room illumination and each procedure lasted approximately 8 to 10 minutes.
Results
The sensitivity maps of the two visual fields performed with two vertex distances can be seen in Figure 3.
The visual field with a 12 mm vertex distance (right side figure) shows the expected circular loss of sensitivity at approximately 12°.
Instead, the 6 mm vertex distance visual field shows an almost normal visual field with scarce loss of sensitivity outside 15° from the fovea (left side figure).
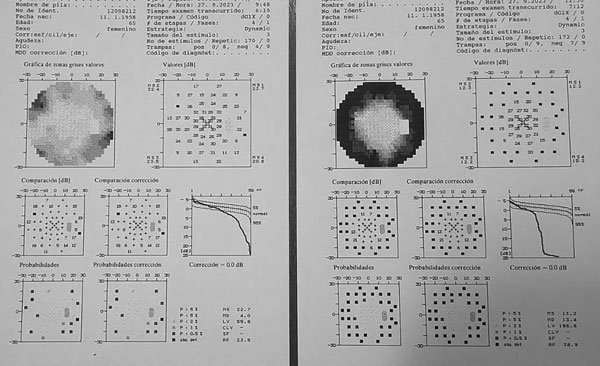
Figure 3. Visual fields of a 60 years-old subject performed with a trial lenses holder with an 8 mm central hole, located at 6 mm (left) and 12 mm (right) vertex distances.
Discussion
The present study shows the projection of a circular shadow in the visual field produced by a trial probe, with an opaque circular zone around a central 8 mm diameter central hole, placed in front of the eye. This study shows that the stimulation of the sensitive area necessary for the effectiveness of defocus systems in myopia can be obtained at a usual vertex distance of 12 mm and that stimulation goes beyond the sensitive area when the vertex distance is reduced to 6 mm. To our knowledge, the vertex distance of tight-fitting myopia control glasses has not yet been considered in clinical trials on myopia progression in children16.
A previous study by using multifocal electroretinogram showed that the most sensitive zone to detect blur is the retina surrounding the fovea at 6 to 12° radius from the optical axis10. The present study shows that a normal vertex distance of 12 mm produces a better treatment area than a 6 mm vertex distance. In fact, even with an 8 mm diameter for the distance vision and a 12 mm vertex distance, the treatment area falls at 10-12° of radius around the optical axis according to the results of the visual field testing in our study. With an OCT camera we have shown similar results for a 8-9 mm optical diameter for distance vision in different myopia control spectacles15, with the defocus zones projecting shadows at the retinal plane in the zones that actually detect defocus with greatest accuracy (Fig. 4). Centering the correct frames for these myopia control spectacles is also crucial for adaptation to these spectacles17.
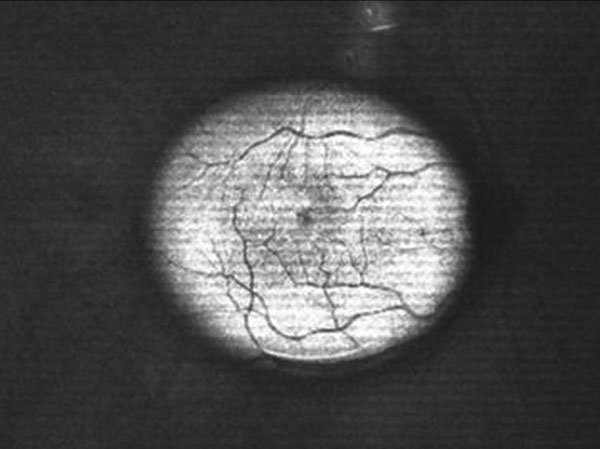
Figure 4. Fundus OCT photograph showing a defocused area around 10° from the fovea with a 8-9 mm center for distance defocus spectacle for myopia control (Myofix, Novar). The papilla and the defocused vessels in the arcades can be seen blurred.
Vertex distance can vary according to age, ethnicity and frame adaptation18. Children younger than 12 have smaller noses with shorter vertex distances. It is also well known that Chinese children have shorter vertex distance than Caucasians. Thus, frame adaptation is crucial as many children may use their spectacles inadequately (downwards and far from the eyes). Inadequate use may contribute for differences in effectivity of myopia control spectacles as the treatment area at the fundus of the eye would vary accordingly.
Conclusion
The present study suggests that vertex distance should be rigorously monitored in myopia control practice and research.
References
1. Lam CSY, Tang WC, Zhang HY, et al. Long-term myopia control effect and safety in children wearing DIMS spectacle lenses for 6 years. Sci Rep 2023; 13(1): 5475. Published 2023 Apr 4. doi:10.1038/s41598-023-32700-7.
2. Bao J, Huang Y, Li X, et al. Spectacle lenses with aspherical lenslets for myopia control vs single-vision spectacle lenses: a randomized clinical trial. JAMA Ophthalmol 2022; 140(5): 472-478. doi:10.1001/jamaophthalmol.2022.0401.
3. Rappon J, Chung C, Young G, et al. Control of myopia using diffusion optics spectacle lenses: 12-month results of a randomised controlled, efficacy and safety study (CYPRESS). Br J Ophthalmol 2023; 107(11): 1709-1715. doi:10.1136/bjo-2021-321005.
4. Iribarren R, Szeps A, Kotlik C, Laurencio L, De Tomas M, Impagliazzo R, Martin G. Short-term axial length changes in myopic eyes induced by defocus spectacles for myopia control. Photonics 2023; 10: 668. doi:10.3390/photonics10060668
5. Alvarez-Peregrina C, Sanchez-Tena MA, Martinez-Perez C, Villa-Collar C; Clinical evaluation of MyoCare in Europe –the CEME Study Group, Ohlendorf A. Clinical Evaluation of MyoCare in Europe (CEME): study protocol for a prospective, multicenter, randomized, double-blinded, and controlled clinical trial. Trials 2023; 24(1): 674. Published 2023 Oct 17. doi:10.1186/s13063-023-07696-0.
6. Tarutta EP, Proskurina OV, Tarasova NA, et al. [Long-term results of perifocal defocus spectacle lens correction in children with progressive myopia]. Vestn Oftalmol 2019; 135(5): 46-53 [article in Russian].
7. Yuval C, Otzem C, Laura BS, et al. Evaluating the effect of a myopia control spectacle lens among children in Israel: 12-month results [published correction appears in Am J Ophthalmol. 2024 Mar;259:197. doi: 10.1016/j.ajo.2023.12.015]. Am J Ophthalmol 2024; 257: 103-112. doi:10.1016/j.ajo.2023.08.019.
8. Schaeffel F, Swiatczak B. Functional changes in the myopic retina interfere with emmetropization. Acta Ophthalmol 2024; 102(S279). Special issue: Abstracts from the 2023 European Association for Vision and Eye Research Festival, 26‐28 October 2023, Valencia, Spain. doi:10.1111/aos.16265.
9. Swiatczak B, Schaeffel F. Myopia: why the retina stops inhibiting eye growth. Sci Rep 2022; 12(1): 21704. Published 2022 Dec 15. doi:10.1038/s41598-022-26323-7.
10. Panorgias A, Aigbe S, Jeong E, Otero C, Bex PJ, Vera-Diaz FA. Retinal responses to simulated optical blur using a novel dead leaves ERG stimulus. Invest Ophthalmol Vis Sci 2021; 62(10): 1. doi:10.1167/iovs.62.10.1.
11. Smith EL 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF. Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci 2005; 46(11): 3965-3972. doi:10.1167/iovs.05-0445.
12. Smith EL 3rd, Campbell MC, Irving E. Does peripheral retinal input explain the promising myopia control effects of corneal reshaping therapy (CRT or ortho-K) & multifocal soft contact lenses? Ophthalmic Physiol Opt 2013; 33(3): 379-384. doi:10.1111/opo.12060.
13. Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology 2011; 118(6): 1152-1161. doi:10.1016/j.ophtha.2010.10.035.
14. Lam CSY, Tang WC, Tse DY, et al. Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol 2020; 104(3): 363-368. doi:10.1136/bjophthalmol-2018-313739.
15. de Tomas M, Szeps A, Martín G, et al. Retinal shadows produced by myopia control spectacles. Ophthalmic Physiol Opt 2024; 44(1): 214-218. doi:10.1111/opo.13228.
16. Wolffsohn JS, Kollbaum PS, Berntsen DA, et al. IMI: clinical myopia control trials and instrumentation report. Invest Ophthalmol Vis Sci 2019; 60(3): M132-M160. doi:10.1167/iovs.18-25955.
17. Szeps A, De Tomas M, Kotlik C, Iribarren R. Axial length changes with diffusion optics multiple segments (DOMS) spectacles for myopia control. Oftalmol Clin Exp 2023; 16(2):148-154. doi:10.70313/2718.7446.v16.n02.228
18. Thompson AJ. Paediatric facial anthropometry applied to spectacle frame design [thesis]. Birmingham UK: Aston University, 2021. https://research.aston.ac.uk/en/studentTheses/paediatric-facial-anthropometry-applied-to-spectacle-frame-design