SURGICAL TECHNIQUES
Staining with trypan blue and retroiridian synechiolysis: effective approach in cataract surgery for patients with chronic uveitis, severe miosis, and posterior synechiae
Andrés Germán Alza
Clínica Privada de Ojos Dr. Enrique Alza, La Plata, Argentina.
Oftalmol Clin Exp (ISSNe 1851-2658)
2024; 17(3): e464-e472.
Though everything has an end, the one thing they cannot take away from you, and that will endure over time, is the ability to share your knowledge.
Abstract
The novel technique of “staining and retroiridian synechiolysis” emerges as an effective alternative to overcome challenges associated with anterior capsular staining and pupillary synechiolysis in patients with chronic uveitis, characterized by severe miosis and posterior synechiae. This technique involves initially performing a minimal peripheral iridectomy to access the retroiridian space and injecting trypan blue for complete staining of the anterior lens capsule. Subsequently, viscoelastic is applied in the anterior chamber, and synechiolysis is performed using an iris repository spatula through the iridectomy site, effectively reducing surgical time. The successful implementation of this technique has facilitated uncomplicated surgery initiation, demonstrating its potential as a viable alternative for these challenging cases.
Keywords: cataract, chronic uveitis, retroiridian space, trypan blue staining, synechiolysis, surgical time.
Tinción con azul tripán y sinequiólisis retroiridiana: abordaje eficaz de la cirugía de cataratas en pacientes con uveítis crónica, miosis intensa y sinequias posteriores
Resumen
La novedosa técnica de “tinción y sinequiólisis retroiridiana” surge como una alternativa eficaz para superar las dificultades asociadas con la tinción capsular anterior y la sinequiólisis pupilar en pacientes con uveítis crónica, caracterizada por miosis intensa y sinequias posteriores. Esta técnica implica realizar inicialmente una iridectomía periférica mínima para acceder al espacio retroiridiano e inyectar azul tripán para lograr una tinción completa de la cápsula anterior del cristalino. Luego se aplica viscoelástico en la cámara anterior y se lleva a cabo la sinequiólisis mediante una espátula repositora de iris a través del sitio de la iridectomía, lo que contribuye a reducir eficazmente el tiempo quirúrgico. La implementación exitosa de esta técnica ha facilitado el inicio de la cirugía sin complicaciones, demostrando su potencial como una alternativa viable para estos casos desafiantes.
Palabras clave: catarata, uveítis crónica, espacio retroiridiano, tinción con azul tripán, sinequiólisis, tiempo quirúrgico.
Introduction
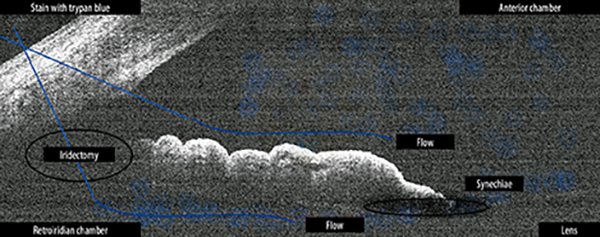
Cataract is a common complication in chronic uveitis, attributed to both inflammation and corticosteroid treatment. Surgery is essential for restoring vision and enabling evaluation and treatment of the posterior segment. However, chronic inflammation of the uvea poses significant challenges in conventional cataract surgery procedures, as documented by Ram et al.1. In the case presented, chronic uveitis caused severe miosis with posterior synechiae affecting the pupil. Challenges in staining the anterior lens capsule and efficiently performing synechiolysis, while minimizing surgical time, were addressed through the “staining and retroiridian synechiolysis” technique (Fig. 1). This innovative technique allows for overcoming these challenges by means of a permeable peripheral iridectomy, in addition to preventing potential postoperative pupil blockages1-2.
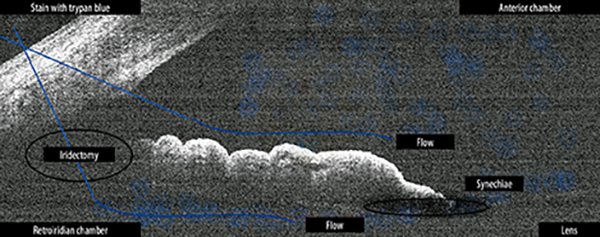
Figure 1. Technique called “retroiridian staining and synechiolysis”.
Case presentation
A case is described of a 75-year-old patient with chronic uveitis and advanced cataract in the left eye (Figs. 2-3). He was referred to our center to undergo cataract phacoemulsification. Several preliminary studies were conducted, including slit-lamp biomicroscopy, which detailed the findings described in Table 1; contact echometry, which reported a narrow anterior chamber and a thickened lens (Fig. 4); ocular ultrasound, which showed a clear vitreous without echoes (Fig. 5); and bilateral ocular response analyzer. According to the study, ocular pressure measured with the Goldmann tonometer is higher in the right eye. But in the left eye, the corrected intraocular pressure is higher and the corneal hysteresis is lower. This is due to higher ocular pressure and corneal edema compared to the right eye (Fig. 6).
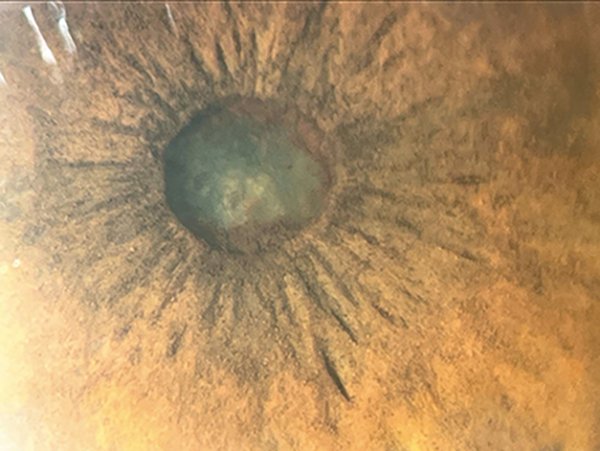
Figure 2. Chronic uveitis, intense miosis, and posterior pupillary synechiae (image captured with the OCUFYTMWIDE device).
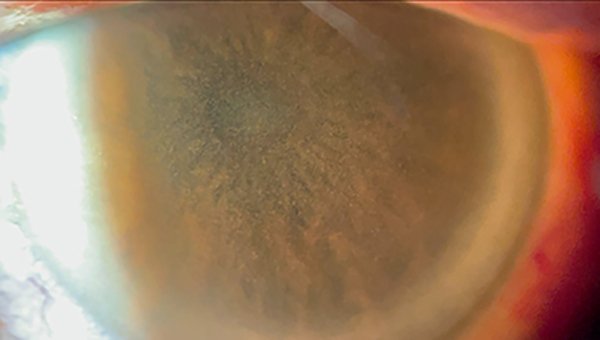
Figure 3. Mild edema, low endothelial cell count, and abundant pigmented endothelial deposits (image captured with the OCUFYTMWIDE device).
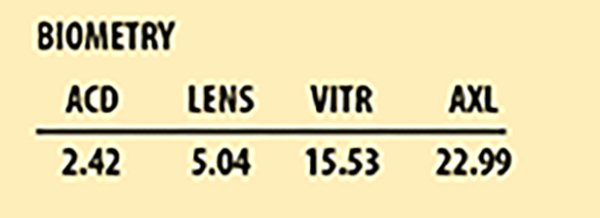
Figure 4. Contact biometry showing narrow anterior chamber and thickened crystalline lens.
Figure 5. Ocular ultrasound: no posterior pole involvement observed.
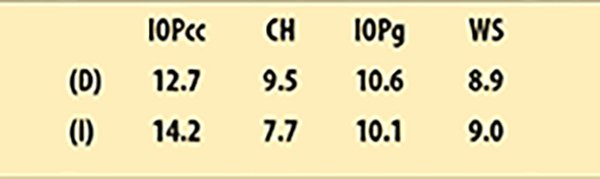
Figure 6. Bilateral ocular response analyzer information. According to the study, ocular pressure measured with the Goldmann tonometer is higher in the right eye. But in the left eye, the corrected intraocular pressure is higher and the corneal hysteresis is lower.
Surgical technique
Preparation
A drop of 5% phenylephrine combined with 0.5% tropicamide was applied to the lower conjunctival sac every 15 minutes, starting 2 hours before surgery. Sub-Tenons anesthesia was administered using a curved Stevens 19G cannula loaded with a mixture of 0.75 ml 1% lidocaine and 0.75 ml 0.5% bupivacaine, both preservative-free.
Incision
The main incision was made with a 2.8-millimeter angled-tip blade. Abundant dilating (DS) solution of 1% lidocaine without preservatives was administered in a 1:2 dilution with Ringer’s lactate solution, plus a 1 ml ampoule of 1‰ adrenaline in 9 ml preservative-free Ringer’s lactate solution diluted 1:10 in the intracameral space.
Retroiridian staining
A small peripheral iridectomy of small diameter was created using Westcott scissors and a Castroviejo toothed forceps of 0.12 mm (Fig. 7) to access the retroiridian space. Additional DS was administered to form the anterior chamber. Trypan blue was injected into the anterior chamber and retroiridian space through the peripheral iridectomy using a 25G spatulated cannula, allowing it to act for a few seconds (Fig. 8). Additional DS was administered to form the anterior chamber and wash the trypan blue.

Figure 7. A small-diameter peripheral iridotomy was created to access the retroiridian space using Westcott scissors and a 0.12 mm Castroviejo toothed forceps.
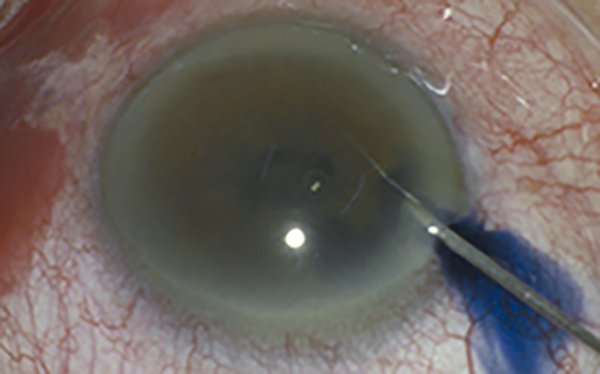
Figure 8. Trypan blue solution was administered into the anterior chamber and retroiridian space through the peripheral iridectomy using a spatulated cannula, allowing it to act for a few seconds.
Retroiridian synechiolysis
Subsequently, 3% sodium hyaluronate viscoelastic solution was applied. The iridectomy provided access to the retroiridian space for synechiolysis and release of pupillary occlusion using a 2.0 mm Culler iris repository spatula (Fig. 9).
Completion of surgery
The remainder of the surgery proceeded with conventional phacoemulsification involving continuous capsulorhexis, using a preloaded 12 mm capsular tension ring and a foldable hydrophilic intraocular lens (Figs. 10-12).

Figure 9. The iridectomy provided access to the retroiridian space, facilitating synechiolysis and pupillary release with the 2.0 mm Culler iris repository spatula.
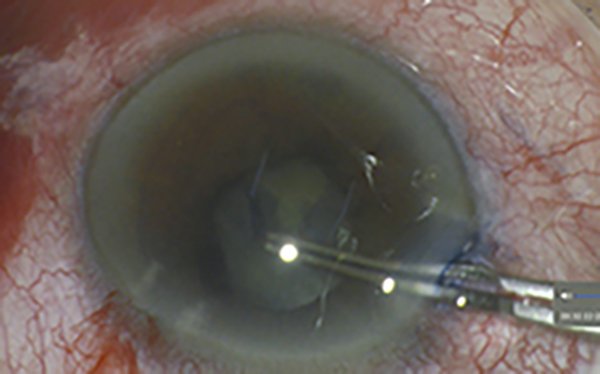
Figure 10. Controlled continuous capsulorhexis.
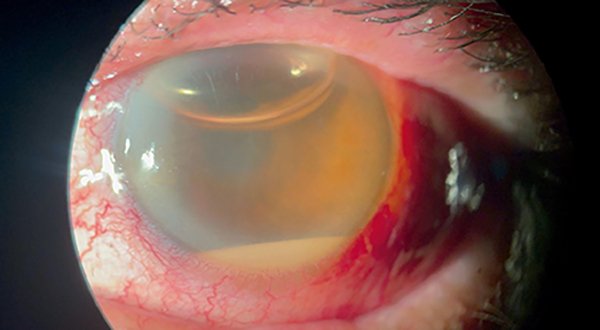
Figure 11. Surgical result at 24 hours (image captured with the OCUFYTMWIDE device).

Figura 12. Postoperative result at 10 days.
Observations
Peripheral iridectomy serves as a pathway to administer trypan blue and facilitate synechiolysis, thereby reducing surgical times. Peripheral iridectomy is useful in preventing potential inflammatory blockages.
Discussion
Cataract surgery in patients with chronic uveitis poses significant challenges due to persistent ocular inflammation. This condition increases the risk of complications. However, experienced anterior segment surgeons can overcome these obstacles using specific techniques, such as the behind-the-iris approach described in the literature3-4. The presence of inflammatory cells and proteins in the aqueous humor promotes the formation of posterior synechiae, which are adhesions between the iris and the anterior capsule of the lens, or between the vitreous in aphakic eyes. These synechiae can also form over certain types of intraocular lenses5. Common difficulties during surgery include incomplete staining of the anterior lens capsule, complicated synechiolysis, and prolonged surgical time. To address these challenges, the technique of “retroiridian staining and synechiolysis” has been developed, which provides an effective solution for capsule staining, synechiae release, and prevention of posterior pupillary blockage (Table 2)2. In this specific context, the “retroiridian staining and synechiolysis” technique has proven to be a valuable tool for overcoming the challenges of cataract surgery in patients with chronic uveitis. The successful implementation of this technique has allowed surgery to be completed without complications, underscoring its effectiveness in this complex clinical environment (Table 3).
Table 1. Findings in the left eye ophthalmological examination.
Exam under slit lamp biomicroscopy |
|
|
|
|
|
|
|
|
|
|
Table 2. Technique of “retroiridian staining and synechiolysis”.
FOUR STEPS PROCEDURE |
Step 1: Peripheral iridectomy |
A small incision is made at the periphery of the iris to access the retro-iridian space. |
|
Step 2: Staining with trypan blue |
|
Trypan blue is injected using a spatulated cannula through the peripheral iridectomy to fully stain the anterior lens capsule. |
|
Step 3: Application of viscoelastic in the anterior chamber |
|
Viscoelastic is applied in the anterior chamber to maintain depth. |
|
Step 4: Synechiolysis |
|
An iris repositor spatula is used to release synechiae through the peripheral iridectomy. |
Table 3. Advantages of “staining and retroiridian synechiolysis” technique.
ADVANTAGES |
Prophylaxis of postoperative pupillary block: peripheral iridectomy prevents inflammatory pupillary block that may occur after surgery. |
Complete staining of the anterior lens capsule: trypan blue diffuses more easily towards the iris periphery, allowing for complete and homogeneous staining, and facilitating capsule visualization during surgery. |
More comfortable and efficient synechiolysis: peripheral iridectomy facilitates access to the retroiridian space, allowing precise and effective release of synechiae behind the iris. |
Reduction of complication risks: working with a fully stained anterior capsule reduces risks of uncontrolled tears and other intraoperative complications. |
Decrease in surgical time: this technique enables simpler and more complete capsule staining in less time, thereby reducing total surgery time. |
Minimization of iris trauma: iris manipulation is minimized by performing the procedure through peripheral iridectomy and reducing surgical times. |
ADDITIONAL BENEFITS |
Prevention of anterior lens capsule impermeabilization: injecting trypan blue before viscoelastic prevents the latter from impermeabilizing the capsule and complicating staining. |
Reduction of endothelial cell loss: performing the procedure through peripheral iridectomy rather than the pupillary margin minimizes the risk of anterior chamber collapse, thereby reducing endothelial cell loss. |
Conclusion
Cataract surgery in patients with chronic uveitis, especially when accompanied by intense miosis and posterior synechiae, poses significant challenges such as incomplete staining of the anterior lens capsule, difficult synechiolysis, and prolonged surgical time. To overcome these obstacles, the technique of “retroiridian staining and synechiolysis” has been developed. This innovative technique involves minimal peripheral iridectomy to access the retroiridian space, followed by injection of trypan blue to ensure complete and uniform staining. Subsequently, viscoelastic material is administered in the anterior chamber, and synechiolysis is performed using an iris repositor spatula through the peripheral iridectomy. This technique represents a novel, safe, and effective alternative to improve outcomes in these challenging cases. Anticipated future studies with a broader case series and long-term follow-up are expected to validate its long-term efficacy.
References
1. Ram J, Gupta A, Kumar S et al. Phacoemulsification with intraocular lens implantation in patients with uveitis. J Cataract Refract Surg 2010; 36: 1283-1288.
2. Vajpayee RB, Angra SK, Titiyal JS et al. Pseudophakic pupillary-block glaucoma in children. Am J Ophthalmol 1991; 111: 715-718.
3. Alza AG, Galletto E. Retroiridian pupilloplasty. Oftalmol Clin Exp 2022; 15: 40-47.
4. Alza AG. Retroiridian anterior vitrectomy: a novel technique for the removal of late cortical remnants located in the posterior segment for anterior segment surgeons. Oftalmol Clin Exp 2024; 17: e128-e133.
5. Moorthy RS, Mermoud A, Baerveldt G et al. Glaucoma associated with uveitis. Surv Ophthalmol 1997; 41: 361-394.