
CLINICAL CASES
Ocular surface complications secondary to eyelid resection of infiltrating basal cell carcinoma
Alberto De Robles Fregoso
Hospital Regional Dr. Valentín Gómez Farías, Zapopan, Jalisco, México.
Oftalmol Clin Exp (ISSNe 1851-2658)
2024; 17(3): e418-e425.
DOI:10.70313/2718.7446.v17.n03.351
Abstract
A 77-year-old female patient with the presence of a cutaneous neoformation of approximately 1 cm by 1 cm was verified at the level of the middle third and external third of the right lower palpebral eyelid, which extended to the tarsal conjunctiva of the fornix. It was decided to perform closed dacryointubation with silicone tube placement, full thickness resection of the lesion with free edges, cheek and preauricular skin rotation flap (Mustardé type) associated with autologous chondro-perichondral graft of the external ear (Matsuo type), with oral mucosa graft to restore the posterior lamella. After 15 days, the patient reports a foreign body sensation at the level of the right eye. irregularity and malposition of the lower eyelid edge, positioning abnormality of the cutaneous mucosal junction line, conjunctival hyperemia, tear breakup time of 5 seconds, tear meniscus measurement of 0.3 mm and 0.5 mm, inferior punctate epithelial keratopathy, which stains with fluorescein.
Keywords: dacryointubation, Mustardé type, infiltrating basal cell carcinoma, iatrogenic lagophthalmos.
Complicaciones de la superficie ocular secundarias a resección de carcinoma basocelular infiltrante
Resumen
Paciente femenina de 77 años con la presencia de una neoformación cutánea de aproximadamente 1 x 1 cm. Se comprobó a nivel del tercio medio y tercio externo del párpado palpebral inferior derecho que se extendía hasta la conjuntiva tarsal del fórnix.
Se decidió realizar dacriointubación cerrada con colocación de tubo de silicona, resección de espesor total de la lesión con bordes libres, mejilla y colgajo de rotación de piel preauricular (tipo Mustardé) asociado a injerto condropericondral autólogo del oído externo (tipo Matsuo), con injerto de mucosa oral para restaurar la laminilla posterior. Después de 15 días la paciente refirió sensación de cuerpo extraño en ojo derecho. Se observó irregularidad y malposición del borde del párpado inferior, anomalía de posicionamiento de la línea de unión de la mucosa cutánea, hiperemia conjuntival, tiempo de ruptura lagrimal de 5 segundos, medición del menisco lagrimal de 0,3 mm y 0,5 mm, queratopatía epitelial puntiforme inferior, que se tiñe con fluoresceína.
Palabras clave: dacriointubación, tipo Mustardé, carcinoma basocelular infiltrante, lagoftalmos iatrogénico.
Complicações da superfície ocular secundárias à ressecção de carcinoma basocelular infiltrante
Resumo
Paciente do sexo feminino, 77 anos, com presença de neoformação cutânea de aproximadamente 1 x 1 cm. Foi confirmado ao nível do terço médio e terço externo da pálpebra palpebral inferior direita que se estendia até a conjuntiva tarsal do fórnice. Optou-se por realizar dacriointubação fechada com colocação de tubo de silicone, ressecção de espessura total da lesão com bordas livres, bochecha e retalho de rotação de pele pré-auricular (tipo Mustardé) associado a enxerto condropericondral autólogo de orelha externa (tipo Matsuo), com enxerto da mucosa oral para restaurar a lamela posterior. Após 15 dias, o paciente relatou sensação de corpo estranho em olho direito. Foram observadas irregularidade e mau posicionamento da borda palpebral inferior, alteração de posicionamento da linha de junção da mucosa cutânea, hiperemia conjuntival, tempo de ruptura lacrimal de 5 segundos, medição do menisco lacrimal de 0,3 mm e 0,5 mm, ceratopatia epitelial puntiforme inferior, corada com fluoresceína.
Palavras-chave: dacriointubação, tipo Mustardé, carcinoma basocelular infiltrante, lagoftalmo iatrogênico.
Introduction
The eyelid and orbital region are topographic areas with great anatomical complexity, and this probably makes be one of the most difficult areas to rebuild in surgery. The tumor disease that most frequently develops in the eyelids are basal cell carcinomas, and are most often found on the eyelid lower. In addition, one must have considered the possibility of spread of these tumors to deeper structures through lines of embryonic fusion of the inner canthus. The fundamental objective of this surgery is, as always, surgery oncology, in the complete exeresis of the tumor lesion, performing conventional excisional surgery or microscopically controlled surgery. Later, in the reconstruction, attempts should be made to preserve eyelid function as much as possible and, finally, to achieve the best result aesthetic possible. Complications like ectropion, corneal exposure, loss of rigidity of the lid margin, lagophthalmos, epiphora or loss of upper eyelid tension may develop in these patients1.
Exposure keratopathy is due to incomplete closure of the eyelids (lagophthalmos), incomplete closure results in poor tear film replenishment, increased tear evaporation, disruption of the mucin layer, corneal drying, and ocular surface breakdown. The term lagophthalmos comes from the Greek word for hare (lagos) because rabbits were thought to sleep with their eyes open. Inability to close the eyelids completely can result from a forward projection of the eye within the orbit, vertical shortening of the upper or lower eyelids, dysfunction of the protractor orbicularis oculi muscle or its seventh cranial nerve motor innervation, or adhesions between the globe and upper lid that limit full eyelid excursion2.
Patients complain of irritation, foreign body sensation, and burning. Slit lamp examination characteristically reveals interpalpebral punctate epithelial keratopathy, which is diagnostic of lagophthalmos. In patients with nocturnal lagophthalmos, the distribution of the punctate epithelial keratopathy will depend on the position of the cornea during sleep. Keratopathy may be inferior, central, or even superior, as some patients have been reported to sleep with the globe depressed. Testing for Bell’s phenomenon has been a fairly poor predictor of actual globe position during sleep2.
External examination for complete lid closure should be done with the patient gently pressing the lids closed, because subtle degrees of lagophthalmos may not be apparent if the lids are forcefully’ squeezed. Acute seventh-nerve dysfunction, due to Bell’s palsy or following trauma or iatrogenic injury, is probably the most frequent cause of lagophthalmos presented to the ophthalmologist. Vertical shortening usually occurs from accidental or iatrogenic trauma due to scarring or over excision of the eyelid skin3.
The purpose of treating lagophthalmos is two-fold: to prevent further corneal exposure and to improve eyelid function. Treatment can be divided into medical and surgical modalities. Medical treatment consists of improving the quantity, quality, and stability of the tear film. Surgical procedures can be dynamic or static and focus on reestablishing eyelid function or eyelid coverage. The choice of treatment and reconstruction method will depend on the location, severity, etiology of lagophthalmos, as well as patient factors of age, health, and their expectations4.
The objective of this work is to present a case of exposure keratopathy in a patient with iatrogenic lagophthalmos secondary to eyelid resection of infiltrating basal cell carcinoma.
Case report
A 77-year-old female patient began her condition 5 years ago with the presence of a lesion on the lower right eyelid, with a papular appearance, which progressively increased in size until it affected almost the entire lower right eyelid.
The presence of a cutaneous neoformation of approximately 1 cm by 1 cm was verified at the level of the middle third and external third of the right lower palpebral eyelid, which extended to the tarsal conjunctiva of the fornix (Fig. 1).

Figure 1. Infiltrating basal cell carcinoma of the lower eyelid margin.
A histopathological study of a skin biopsy obtained from the cutaneous neoformation was carried out, which reported epidermis with ulceration, dermis with numerous neoplastic basaloid cells, which in some areas formed accumulations with peripheral palisades and infiltrating cords in other areas. Dilated blood vessels, lymphocytic inflammatory infiltrate and solar elastosis are observed, findings compatible with an infiltrating basal cell carcinoma.
It was decided to perform closed dacryo-intubation with silicone tube placement, full thickness resection of the lesion with free edges, cheek and preauricular skin rotation flap (Mustardé type) (Figs. 2 to 5) associated with autologous chondro-perichondral graft of the external ear (Matsuo type), with oral mucosa graft to restore the posterior lamella (Figs. 6 to 8).
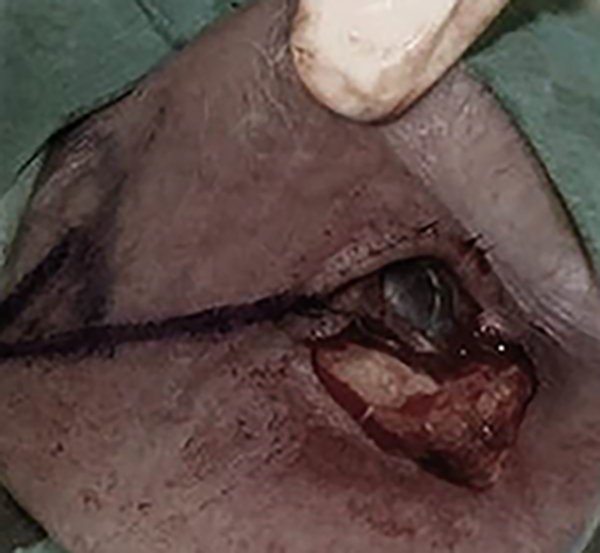
Figure 2. Full thickness block V resection with defect greater than half of the lower eyelid.
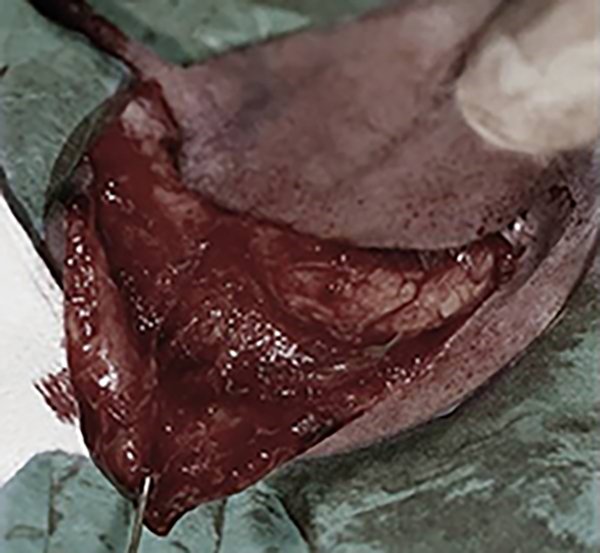
Figure 3. Cantholysis and advancement flap.

Figure 4. Post-operative results cheek and preauricular skin rotation flap (Mustarde type).

Figure 5. Post-operative results cheek and preauricular skin rotation flap (Mustarde type).

Figure 6. Post-operative results autologous chondro-perichondral graft of the external ear (Matsuo type) and oral mucosa graft.

Figure 7. Oral mucosa graft donor site.

Figure 8. Chondro-perichondral graft of the external ear donor site.
The histopathological study of a 2 cm by 2 cm skin spindle, with 2 cm subcutaneous cell tissue, reported a fibrous lesion with solar elastosis, ecstatic and glandular changes, as well as reactive and inflammatory adnexal and no evidence of basal cell neoplasia.
After 15 days, the patient reports a foreign body sensation at the level of the right eye. The external examination shows incomplete palpebral closure with exposure of the bulbar conjunctiva and lower eyelid retraction (Figs. 9 and 10).

Figure 9. Incomplete palpebral closure with exposure of the bulbar conjunctiva and lower eyelid retraction.

Figure 10. Incomplete palpebral closure with exposure of the bulbar conjunctiva and lower eyelid retraction.
Slit-lamp examination right eye reveals irregularity and malposition of the lower eyelid edge, positioning abnormality of the cutaneous mucosal junction line, conjunctival hyperemia, tear breakup time of 5 seconds, tear meniscus measurement of 0.3 mm and 0.5 mm, inferior punctate epithelial keratopathy, which stains with fluorescein (Figs. 11 and 12).

Figure 11. Inferior punctate epithelial keratopathy.

Figure 12. Irregularity and malposition of the lower eyelid edge.
It was decided to initiate a conservative management of the corneal affection by means of the application of 3% trehalose ophthalmic solution with 0.15% sodium hyaluronate every 2 hours, Carbomer ophthalmic gel 2 mg/gr every 8 hours and palpebral massage, reassessing the patient.
After 2 months, improvement was obtained regarding the symptoms, tear breakup time of 10 seconds, tear meniscus measurement of 0.8 mm and 0.9 mm cornea with uniform epithelialization was observed, without staining with fluorescein, as well as a decrease in conjunctival exposure at eyelid closure (Figs. 13 and 14), it is decided to remove the dacryo-intubation probe.
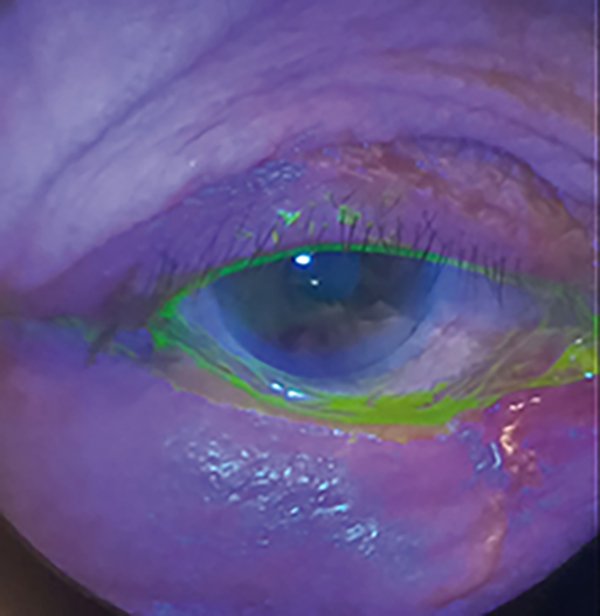
Figure 13. Remission of the inferior punctate epithelial keratopathy.

Figure 14. Decrease in conjunctival exposure when closing the eyelid.
Discussion
The techniques to be used for both upper and lower eyelid reconstruction are multiple, and their choice will depend largely on the magnitude of the defect created and its location, as well as the histology of the lesion and other aspects such as the age of the patients3.
The closure of defects in the lower eyelid aims to reconstruct the anterior lamella of the eyelid. The wound tension should be directed parallel to the eyelid margin to avoid subsequent complications, such as ectropion or scar retraction. Incisions and closure lines should follow the natural contour lines periocular, so that they hide between them5.
The most important flaps in this region are rectangular advancement, rotational and translational. In our case we selected the Mustardé flap It is an advancement and rotation flap of the lower cheek that allows reconstruction very severe defects of almost the entire extension of the lower eyelid, either alone or associated with any posterior lamella support graft5.
As in the reconstruction of lower eyelid defects, until the 25%-33% of the total size of the upper eyelid can be closed by closure straight. Severe upper eyelid defects that cannot be addressed. By conventional techniques they can be solved through a flap pedunculated margin of the lower eyelid including the marginal artery (a 3 or 4 mm from the edge) and then transferred in a two-step procedure stages. It is the so-called Cutler-Beard flap5.
The inner canthus is an area considered high risk in tumor management because it is a centrofacial, periorificial and fusion area embryonic. In the reconstruction of this area it is essential to try to preserve, in the As much as possible, the lacrimal duct trying to tutor it during surgery, the most used are the advancement and rotation ones5.
Preserving the function of the eyelid as much as possible is one of the most important objectives in eyelid surgery, trying to preserve the function as much as possible tear drainage and eye protection that they provide1.
To do this, some complications must be avoided such as entropion, ectropion, lagophthalmos, epiphora and corneal exposure. Lagophthalmos is impossibility to completely close the eyelids, with the consequent corneal exposure and risk of keratitis as is the case of our patient1.
Management of lagophthalmos involves both medical and surgical approaches with the aim of treating the underlying condition leading to exposure keratopathy and protection of the ocular surface4.
Artificial tears without preservatives can be administered frequently in order to improve the patient’s tear film. The ointment can be applied at night time or during the day if there is severe corneal exposure. Taping of the eyelids at night can offer additional ocular surface protection without resorting to surgery. There are also moisture chamber-type glasses which can aid in maintaining a stable tear film and improve symptoms. The volumizing hyaluronic acid gel has been used for tissue expansion for immediate management of cicatricial ectropion in cases of lagophthalmos4.
When there is corneal exposure and recovery is expected within a matter of weeks, a temporary tarsorrhaphy can be a good option. In the majority of cases, the cornea can be protected adequately by closing the lateral one-third of the eyelids. A small opening should remain so that the cornea can be continuously assessed and required topical medications can be administered4.
If there is no full lid closure, gold or platinum weight can be implanted into the upper eyelid in patients with paralytic lagophthalmos. This will result in a gravity-dependent enhancement of eyelid closure. Gold was initially used because it is inert. Platinum has a higher density which translates to a slimmer profile, decreased visibility, and improved cosmesis6.
Lower eyelid laxity occurs in facial nerve paralysis and floppy eyelid syndrome. Lid tightening procedures such as lateral tarsal strip will lead to improved apposition of the lower eyelid to the globe and decrease scleral exposure and epiphora symptoms. If there is persistent corneal exposure after medical therapy and upper eyelid surgery, lower eyelid elevation with retractor muscle recession can be an option. If there are cicatricial changes a full-thickness skin graft and/or mucous membrane graft could be needed7.
Conclusion
There may be an increase in the prevalence of neoplasms at the level of the palpebral margin, which represent a medical and surgical challenge for all ophthalmologists due to the anatomical and functional complexity of the eyelid. Therefore, it is of utmost importance that the surgeon knows not only the management of these injuries, but also masters the reconstructive options without forgetting all the complications associated with these surgical treatments, since these will lead to a low quality of life for our patients, for example. Finally, this work seeks to enhance the concept that the success secret of ocular surface care is “Don’t Forget the Eyelids!”
References
1. Iglesias ME, Santesteban R, Larumbe A. Oncologic surgery of the eyelid and orbital region. Actas Dermosifiliogr 2015; 106: 365-375.
2. Krachmer JH, Mannis MJ, Holland EJ. Cornea. 5th ed. London: Elsevier, 2022.
3. Pfeiffer MJ, Pfeiffer N, Valor C. Estudio descriptivo sobre el carcinoma basocelular en el párpado. Arch Soc Esp Oftalmol 2015; 90: 426-431.
4. Fu L, Patel BC. Lagophthalmos. In: StatPearls [en línea]. Treasure Island (FL): StatPearls Publishing, 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560661/
5. Miranda Rollón MD, Giménez Castejón D, Molero Izquierdo C et al. Manejo de colgajos cutáneos en la cirugía reconstructiva palpebral. Thea Superficie Ocular 2018; 2: 060. Available from: https://www.laboratoriosthea.com/medias/lab-350-0418_v4_web.pdf
6. Manodh P, Devadoss P, Kumar N. Gold weight implantation as a treatment measure for correction of paralytic lagophthalmos. Indian J Dent Res 2011; 22: 181.
7. Rita MRH, Deepa M, Gitanjali VC et al. Lagophthalmos: an etiological lookout to frame the decision for management. Indian J Ophthalmol 2022; 70: 3077-3082.