CLINICAL CASES
Simultaneous bilateral intraocular collamer lens implant in a patient with psychomotor impairment
Ruth Eskenazi-Betech, Guillermo Raúl Vera-Duarte, Gustavo Ortiz-Morales, Arturo Gómez-Bastar, Arturo Ramírez-Miranda, Alejandro Navas, Enrique O. Graue-Hernández
Instituto de Oftalmología Fundación Conde de Valenciana, Mexico City, México.
Oftalmol Clin Exp (ISSNe 1851-2658)
2024; 17(2): e294-e299.
There is no conflict of interest to disclose.
There is no funding received for this work.
Abstract
To report a case of simultaneous bilateral implantable collamer lens (SBICL) implantation in a patient with a history of psychomotor impairment and seizures. A 31-year-old woman and her legal tutor presented to our outpatient department for refractive surgery to correct her high myopia. She had a medical history of premature birth, cerebral stroke at three months old subsequent psychomotor impairment, and seizures and was therefore incapable of using contact lenses. On presentation, the best corrected visual acuity was 20/60 and 20/80 in the right and left eye, respectively for high myopic astigmatism. Slit lamp examination revealed a normal anterior segment and mild fundus alterations related to high myopia. The patient underwent uneventful simultaneous bilateral implantable collamer lens with general anesthesia. No intraoperative or postoperative complications were observed. In certain circumstances, patients might benefit from simultaneous bilateral implantable collamer lens, which has been shown to have an excellent safety profile and is effective in correcting high myopia.
The reluctance of ophthalmologists to contemplate simultaneous bilateral intraocular surgery is due to apprehension that such an approach may generate specific complications, which could culminate in bilateral visual impairment. However, recent advances in surgical safety and efficacy have led to a reevaluation of indications, analogous to the paradigm shift observed in cataract surgery. In certain circumstances, patients with particular characteristics may require general anesthesia, and the benefits versus risks of concurrent bilateral surgery under such anesthesia merit consideration.
Keywords: posterior chamber phakic intraocular lenses, ICL implantable collamer lens, intraocular lenses implantation, refractive surgery, high myopia.
Implante bilateral simultáneo de lente intraocular de colámero en paciente con deterioro psicomotor
Resumen
Reportar un caso de implantación simultánea bilateral de lente fáquica de cámara posterior de colámero en una paciente con antecedentes de deterioro psicomotor y convulsiones. Paciente mujer de 31 años acudió a nuestro servicio para someterse a cirugía refractiva. Contaba con antecedentes médicos de nacimiento prematuro, accidente cerebrovascular a los tres meses de edad, deterioro psicomotor subsiguiente y convulsiones con intolerancia a las lentes de contacto. En el momento de la presentación, la agudeza visual mejor corregida era de 20/60 y 20/80 en el ojo derecho e izquierdo, respectivamente, por astigmatismo miópico alto. El examen con lámpara de hendidura reveló un segmento anterior normal. La paciente fue sometida a la implantación simultánea de la lente de colámero implantable sin incidentes y con anestesia general. No se observaron complicaciones intraoperatorias ni postoperatorias. La reticencia de los oftalmólogos a contemplar la cirugía intraocular bilateral simultánea se debe a la aprensión de que tal enfoque pueda generar complicaciones específicas que podrían culminar en una discapacidad visual bilateral. Sin embargo, los recientes avances en seguridad y eficacia quirúrgica han llevado a reevaluar las indicaciones de forma análoga al cambio de paradigma observado en la cirugía de cataratas. En determinadas circunstancias, los pacientes con características particulares pueden necesitar anestesia general, por lo que los beneficios frente a los riesgos de la cirugía bilateral concurrente bajo dicha anestesia merecen su consideración.
Palabras clave: lentes intraoculares fáquicas de cámara posterior, lente de colámero implantable, cirugía refractiva, miopía alta.
Implante bilateral simultâneo de lente intraocular collamer em paciente com deterioração psicomotora
Resumo
Relatar um caso de implante bilateral simultâneo de lente fácica Collamer de câmara posterior em paciente com história de comprometimento psicomotor e convulsões. Paciente do sexo feminino, 31 anos, procurou nosso serviço para realizar cirurgia refrativa. Ele tinha histórico médico de parto prematuro, acidente vascular cerebral aos três meses de idade, deterioração psicomotora subsequente e convulsões com intolerância a lentes de contato. Na apresentação, a melhor acuidade visual corrigida foi de 20/60 e 20/80 nos olhos direito e esquerdo, respectivamente, por astigmatismo miópico alto. O exame com lâmpada de fenda revelou um segmento anterior normal. O paciente foi submetido ao implante simultâneo da lente Collamer implantável sem incidentes e sob anestesia geral. Não foram observadas complicações intra ou pós-operatórias. A relutância dos oftalmologistas em contemplar a cirurgia intraocular bilateral simultânea deve-se ao receio de que tal abordagem possa levar a complicações específicas que poderiam culminar em deficiência visual bilateral. No entanto, os recentes avanços na segurança e eficácia cirúrgica levaram a uma reavaliação das indicações análoga à mudança de paradigma observada na cirurgia de catarata. Em certas circunstâncias, pacientes com características particulares podem necessitar de anestesia geral, portanto os benefícios versus riscos da cirurgia bilateral concomitante sob tal anestesia merecem consideração.
Palavras-chave: lentes intraoculares fácicas de câmara posterior, lente Collamer implantável, cirurgia refrativa, miopia alta.
Introduction
Refractive error constitutes a prominent etiological factor contributing to reversible visual impairment on a global scale, and corrective refractive surgery stands as one of the most extensively employed ophthalmic surgical procedures worldwide1-3. In patients who require high-power corrections or in those where kerato-refractive surgery is relatively contraindicated, the phakic intraocular lens emerges as a viable and pertinent alternative.
Implantable collamer lenses (ICL) have garnered considerable acclaim and widespread adoption within refractive surgery owing to technological advancements and notable enhancements in outcomes4. ICLs have a history of >10 years showing effectiveness and safety in correcting high myopia4-6. ICL implantation is usually performed as a delayed, bilateral surgery. However, in some particular patients, general anesthesia and a simultaneous bilateral implantable collamer lens (SBICL) can provide benefits in achieving a safe and effective refractive correction. In this case report, we present a patient with psychomotor impairment and seizures who underwent SBICL for correcting high myopia.
Case report
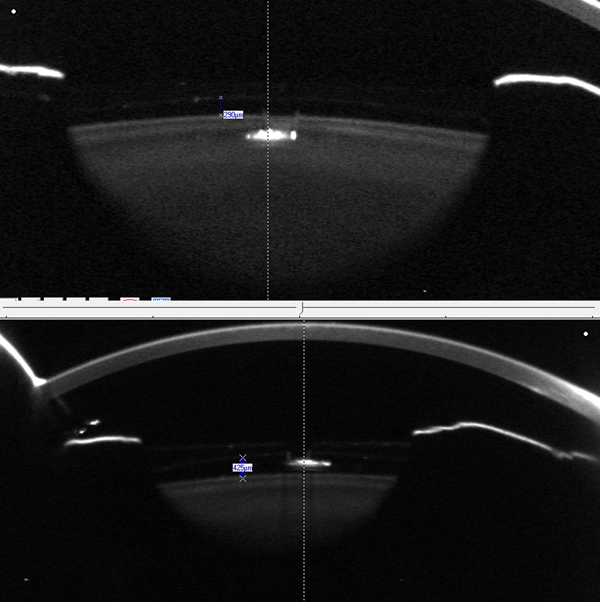
A 31-year-old woman and her legal tutor presented to our outpatient department looking for a solution to correct her high myopia. She had a medical history of premature birth, stroke at 3 months old, and subsequent mental retardation, psychomotor impairment and seizures with intolerance to contact lenses (CL). On presentation, the best corrected visual acuity (BCVA) was 20/60 and 20/80 in the right eye (RE) and left eye (LE), respectively. The manifest refraction in the RE was -11.50=-1.50 X 170 and LE -12.00=-2.50 X 180. The slit lamp examination revealed a normal anterior segment and the fundus examination revealed mild choroidal alterations related to high myopia. The intraocular pressure (IOP) with a rebound tonometer was 14 mm Hg OU. Central corneal thickness (CCT) was 453 µm RE and 442 µm LE. The specular count was 3126 cells/mm2 RE and 2980 cells/mm2 LE. Corneal topography Pentacam camera (Oculus Optikgeräte GmbH, Wetzlar, Germany) and Orbscan (Bausch & Lomb, Rochester, New York) OU revealed steep corneas with a symmetrical bow tie. The posterior elevation maps were within the normal range. The anterior chamber depth measured from the endothelium was 3.17 mm RE and 3.09 mm LE. The white-to-white (WTW) diameters were RE 10.9 mm and LE 10.8 mm. After obtaining signed informed consent and explaining the risks of SBICL, the patient and her legal tutor decided to undergo SBICL under general anesthesia. The patient underwent uneventful SBICL with the V4c ICL (Staar Surgical, Lake Forest, California) simultaneous implantation of ICL (V4c model, RE diopter power -12.50, 12.1 mm and LE diopter power -18.00 +2.50 x 100, 12.1 mm) (Table 1).No intraoperative or postoperative complications were observed during her follow-up of 12 months. After surgery, the patient was very satisfied; she had an uncorrected distance visual acuity (UDVA) of RE 20/40, LE 20/30, and normal IOP. Lens vault in the RE 290 and LE 425 µm (Fig. 1).
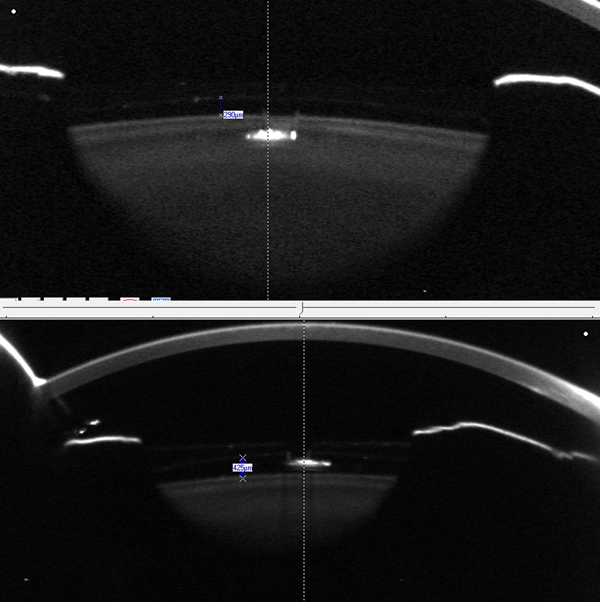
Figure 1. Measurements of the vault by Scheimpflug tomography of an ICL with Aquaport t. A) RE vault 290 µm. B) LE vault 425 µm.
Table 1. Data used for ICL calculation in both eyes.
Right eye (RE) |
Left eye (LE) |
|
Refraction |
-11.50 = -1.50 x 170 |
-12.00 = -2.50 x 180 |
Keratometry (D) |
48.7 / 49.5 |
49.3 / 51.4 |
ACD (mm) |
3.15 |
3.06 |
CCT (µm) |
453 |
442 |
WTW (mm) |
11 |
10.7 |
Recommended ICL |
— |
— |
Abbreviations: ICL: Implantable collamer lens. ACD = anterior chamber depth. CCT: Central corneal thickness. WTW: white to white.
Discussion
Phakic intraocular lenses (pIOLs) have heralded a significant advancement as an alternative approach in addressing myopic patients who are unsuitable candidates for laser vision correction. The Visian implantable collamer lens (ICL, STAAR Surgical Co., Monrovia, CA) is the sole FDA-approved posterior chamber pIOL. While it has demonstrated comparable outcomes concerning safety, efficacy, predictability, and stability, a subset of patients may encounter complications necessitating explanation7. Advantages of pIOLs include a large range of refractive errors, reversible or removable procedures, preserves the natural accommodation, and a lower risk of retinal detachment8. Disadvantages include the potential risk of intraocular surgery, including endophthalmitis, development of iatrogenic cataracts, pupillary block, and endothelial loss9.
Reluctance within a subset of ophthalmologists to consider the prospect of concurrent bilateral surgical procedures is founded on the concern that adopting such an approach could potentially lead to the emergence of distinct complications, ultimately resulting in bilateral visual impairment, an essential example of simultaneous bilateral cataract surgeries10-11. Nevertheless, recent advancements in surgical safety and efficacy prompt a reevaluation of the indications, analogous to the paradigm shift observed in cataract surgery. In certain circumstances, patients with particular characteristics may necessitate general anesthesia, wherein the benefits vis-à-vis risks of concurrent bilateral surgery under such anesthesia warrant consideration.
The main concern about simultaneous surgery is bilateral endophthalmitis12-14, although other bilateral catastrophic complications are also considered, such as expulsive hemorrhage or retinal detachment10, 15-17. To mitigate the risk of endophthalmitis in our patient, a strategy of managing the procedures in each eye as separate consecutive surgeries were performed. The surgical team was well-informed of the need for extra precautions, and a meticulous protocol was established to ensure a systematic transition from the completion of the first eye to the commencement of the second eye, encompassing guidelines on the movement of instruments, their placement, and the sequence of actions. Upon completion of the first eye, the instrument tray was replaced, and all personnel changed gloves before accessing a different set of sterile instruments for the second eye. In addition, a new ophthalmic balanced salt solution and viscoelastic substance were used in the second eye to enhance safety measures further. Before the start of each surgery, a 5% povidone-iodine solution was applied to the lower conjunctival cul-de-sac of both eyes just before the patient was admitted to the operating room and underwent an exhaustive lavage with 10% povidone-iodine both facial areas before each surgery18-19. The incidence of Endophthalmitis after ICL implantation, including infectious endophthalmitis and aseptic endophthalmitis, is about 0.0167%20-21. Other complications include a rise in intraocular pressure (IOP) after the implantation of ICLs, which can be linked to factors like pupillary block, pigment dispersion, and the use of steroids9. Furthermore, reported cases of toxic anterior segment syndrome (TASS) have also been documented22.
The patient exhibited substantial satisfaction with the postoperative improvement in symptoms and vision, as reported by her family, resulting in a transformative change in her lifestyle. Despite inherent communication difficulties, she experienced a renewed sense of exploring and perceiving her surroundings. The refractive challenges encountered during the assessment of visual acuity were surmountable, ultimately yielding more favorable outcomes than initially anticipated. The UCVA exceeded the BCVA before surgery. SBICL implantation presents a viable option for patients with high myopia and psychomotor delay, offering the potential to enhance their quality of life.
Our technique presented discernible advantages, with the simultaneous approach demonstrating superior cost-effectiveness by minimizing the number of procedures, streamlining logistical aspects, and obviating the need for repeated general anesthesia. Although the simultaneous approach incurred a heightened risk of bilateral endophthalmitis, vigilant precautions were taken to mitigate this potential complication. To our knowledge, the current report represents the first documented case of SBICL. We acknowledge that the outcomes of this case report warrant validation through larger-scale series or clinical trials before universal applicability can be ascertained. Nonetheless, our findings offer a novel possibility for optimizing the management of cases where patient cooperation poses a challenge, necessitating specialized care.
References
1. Kim TI, Alió Del Barrio JL, Wilkins M et al. Refractive surgery. Lancet 2019; 393: 2085-2098.
2. Lou L, Yao C, Jin Y et al. Global patterns in health burden of uncorrected refractive error. Invest Ophthalmol Vis Sci 2016; 57: 6271-6277.
3. Naidoo KS, Leasher J, Vision Loss Expert Group of the Global Burden of Disease Study et al. Global vision impairment and blindness due to uncorrected refractive error, 1990-2010. Optom Vis Sci 2016; 93: 227-234.
4. Zhang J, He F, Liu Y, Fan X. Implantable collamer lens with a central hole for residual refractive error correction after corneal refractive surgery. Exp Ther Med 2020; 20: 160.
5. Jiménez-Alfaro I, Gómez-Tellería G, Bueno JL, Puy P. Contrast sensitivity after posterior chamber phakic intraocular lens implantation for high myopia. J Refract Surg 2001; 17: 641-645.
6. Uusitalo RJ, Aine E, Sen NH, Laatikainen L. Implantable contact lens for high myopia. J Cataract Refract Surg 2002; 28: 29-36.
7. AlQahtani BS, Alshamrani AA, Alsulami RE, Vargas JM. A case of implantable collamer lens (ICL) with reverse orientation for 10 years. Case Rep Ophthalmol Med 2021; 2021: 6641475.
8. Nanavaty MA, Daya SM. Refractive lens exchange versus phakic intraocular lenses. Curr Opin Ophthalmol 2012; 23: 54-61.
9. Fernandes P, González-Méijome JM, Madrid-Costa D et al. Implantable collamer posterior chamber intraocular lenses: a review of potential complications. J Refract Surg 2011; 27: 765-776.
10. Arshinoff SA, Strube YN, Yagev R. Simultaneous bilateral cataract surgery. J Cataract Refract Surg 2003; 29: 1281-1291.
11. Sarikkola AU, Kontkanen M, Kivelä T, Laatikainen L. Simultaneous bilateral cataract surgery: a retrospective survey. J Cataract Refract Surg 2004; 30: 1335-1341.
12. Dickman MM, Spekreijse LS, Winkens B et al. Immediate sequential bilateral surgery versus delayed sequential bilateral surgery for cataracts. Cochrane Database Syst Rev 2022; 2022: CD013270.
13. Leivo T, Sarikkola AU, Uusitalo RJ et al. Simultaneous bilateral cataract surgery: economic analysis; Helsinki Simultaneous Bilateral Cataract Surgery Study Report 2. J Cataract Refract Surg 2011; 37: 1003-1008.
14. Ozdek SC, Onaran Z, Gürelik G et al. Bilateral endophthalmitis after simultaneous bilateral cataract surgery. J Cataract Refract Surg 2005; 31: 1261-1262.
15. Mandal AK, Bhatia PG, Gothwal VK et al. Safety and efficacy of simultaneous bilateral primary combined trabeculotomy-trabeculectomy for developmental glaucoma. Indian J Ophthalmol 2002; 50: 13-19.
16. Puvanachandra N, Humphry RC. Bilateral endophthalmitis after bilateral sequential phacoemulsification. J Cataract Refract Surg 2008; 34: 1036-1037.
17. Nallasamy S, Davidson SL, Kuhn I et al. Simultaneous bilateral intraocular surgery in children. J AAPOS 2010; 14: 15-19.
18. Zaharia AC, Dumitrescu OM, Rogoz RE et al. Preoperative antisepsis in ophthalmic surgery (a review). Rom J Ophthalmol 2021; 65: 120-124.
19. Trinavarat A, Atchaneeyasakul LO, Nopmaneejumruslers C, Inson K. Reduction of endophthalmitis rate after cataract surgery with preoperative 5% povidone-iodine. Dermatology 2006; 212 Suppl 1: 35-40.
20. Allan BD, Argeles-Sabate I, Mamalis N. Endophthalmitis rates after implantation of the intraocular collamer lens: survey of users between 1998 and 2006. J Cataract Refract Surg 2009; 35: 766-769.
21. Davis MJ, Epstein RJ, Dennis RF, Cohen JA. Culture-positive endophthalmitis after implantation of intraocular collamer lens. J Cataract Refract Surg 2009; 35: 1826-1828.
22. Eissa SA, Sadek SH, El-Deeb MW. Anterior chamber angle evaluation following phakic posterior chamber collamer lens with CentraFLOW and its correlation with ICL vault and intraocular pressure. J Ophthalmol 2016; 2016: 1383289.