ORIGINAL ARTICLES
Prevalence of myopia, outdoor exposure and screen time at university entrance in Bahía Blanca urban environment
Adriana Cecilia Borellia, Ignacio Buffonea, Ezequiel Jouglardb, Ayelén Méridab, Walter Villalbab, Rafael Iribarrenc-d
aSecretariat of Health of Bahía Blanca, Bahía Blanca, Argentina.
bNational University of the South, Bahía Blanca. Argentina.
cDoctors Iribarren Eye Consultants, Buenos Aires, Argentina.
dRetina Foundation, Buenos Aires, Argentina.
Oftalmol Clin Exp (ISSNe 1851-2658)
2024; 17(2): e189-e197.
Abstract
Objective: Myopia is one of the main causes of spectacle wear in university students. Factors contributing to its development are screen time, reading and outdoor exposure. The aim of this study was to determine the prevalence of myopia in university students in the city of Bahía Blanca, and to establish whether outdoor exposure, screen use and reading are all are related to myopia.
Material and methods: This is a descriptive cross-sectional study. University entrants during 2022 were included. Visual screening and completion of a form was performed to determine outdoor, reading and screen exposure. Those who did not pass the visual acuity test were referred for ophthalmological exam. The prevalence of myopia was calculated and binary logistic regression was used to determine the association of exposure factors.
Results: In all, 413 university students were evaluated with visual acuity testing. A total of 115 students who not passed the visual acuity test, attended for diagnosis, with 95 presenting myopia. The prevalence of myopia was 27.2% (95%CI=22.9-31.5%). The OR for outdoor exposure was less than 1, while for screens and reading it was greater than 1, although the results were not statistically significant.
Conclusion: A moderate prevalence of myopia was demonstrated. Outdoor exposure was high compared to other studies. No association of myopia with exposure factors was found.
Keywords: myopia, outdoor, screens, reading.
Prevalencia de miopía, exposición al aire libre y tiempo de pantalla en el ingreso a la universidad en el entorno urbano de Bahía Blanca
Resumen
Objetivo: La miopía es una de las principales causas de uso de gafas en estudiantes universitarios. Los factores que contribuyen a su desarrollo son el tiempo frente a la pantalla, la lectura y la exposición al aire libre. El objetivo de este estudio fue determinar la prevalencia de miopía en estudiantes universitarios de la ciudad de Bahía Blanca y establecer si la exposición al aire libre, el uso de pantallas y la lectura están relacionados con la miopía.
Material y métodos: Se trata de un estudio descriptivo transversal. Se incluyeron estudiantes que ingresaron en la universidad en 2022. Se realizó un cribado visual y se cumplimentó un formulario para determinar la exposición al aire libre, a la lectura y a pantallas. Los que no superaron la prueba de agudeza visual fueron remitidos a examen oftalmológico. Se calculó la prevalencia de miopía y se utilizó una regresión logística binaria para determinar la asociación de los factores de exposición. Resultados: En total, 413 estudiantes universitarios fueron evaluados con pruebas de agudeza visual. Un total de 115 estudiantes que no superaron la prueba de agudeza visual acudió para diagnóstico, donde 95 presentaron miopía. La prevalencia de miopía fue del 27,2% (IC 95%=22,9-31,5%). La OR para exposición al exterior fue inferior a 1, mientras que para pantallas y lectura fue superior a 1, aunque los resultados no fueron estadísticamente significativos.
Conclusiones: Se demostró una prevalencia moderada de miopía. La exposición al aire libre fue elevada en comparación con otros estudios. No se encontró asociación de la miopía con los factores de exposición.
Palabras clave: miopía, medioambiente, pantallas, lectura.
Prevalência de miopia, exposição externa e tempo de tela no ingresso à universidade no ambiente urbano de Bahía Blanca
Resumo
Objetivo: A miopia é uma das principais causas do uso de óculos em estudantes universitários. Os fatores que contribuem para o seu desenvolvimento são o tempo de tela, a leitura e a exposição ao ar livre. O objetivo deste estudo foi determinar a prevalência da miopia em estudantes universitários da cidade de Bahía Blanca e estabelecer se a exposição ao ar livre, o uso de telas e a leitura estão relacionados à miopia.
Material e métodos: Trata-se de um estudo descritivo transversal. Foram incluídos alunos que ingressaram na universidade em 2022. Foi realizada uma triagem visual e preenchido um formulário para determinar a exposição ao ar livre, leitura e telas. Aqueles que não superaram o teste de acuidade visual foram encaminhados para exame oftalmológico. Calculou-se a prevalência de miopia e utilizou-se regressão logística binária para determinar a associação dos fatores de exposição.
Resultados: No total, 413 universitários foram avaliados com testes de acuidade visual. Compareceram para diagnóstico 115 alunos que não passaram no teste de acuidade visual, onde 95 apresentavam miopia. A prevalência de miopia foi de 27,2% (IC 95%=22,9-31,5%). O OR para exposição ao ar livre foi menor que 1, enquanto para telas e leitura foi maior que 1, embora os resultados não tenham sido estatisticamente significativos.
Conclusões: Foi demonstrada uma prevalência moderada de miopia. A exposição ao ar livre foi alta em comparação com outros estudos. Nenhuma associação de miopia com fatores de exposição foi encontrada.
Palavras-chave: miopia, ambiente, telas, leitura.
Introduction
Myopia is one of the main causes for distance spectacle use in the school and university populations1. Although for years myopia was thought to be genetic in origin, it is now clear that most cases are caused by the environment2-4. The two environmental factors that contribute to its development are the amount of time spent reading or looking at screens, and the amount of outdoor exposure that children and adolescents have3-4. In the 2000s these two factors were discovered5-6, and it has since been confirmed in multiple studies that there are more cases of myopia when children read intensely and when they are not outdoors3. These two environmental factors involve the lifestyle of children and adolescents in a given region, so preventing myopia by inducing lifestyle changes in the population becomes a public health issue that needs medical counselling7.
In this sense, epidemiological work on the prevalence of myopia in several populations started in the 1970s8-10 and has been systematically developed showing a steady increase in prevalence from low figures of 10%-15% in the oldest samples to values of 70%-85% in most recent studies1. The situation of increasing cases is so remarkable that since 2015 the WHO has begun to speak of a “myopia epidemic” and has issued an extensive report on the various public health and medical care approaches needed to curb the epidemic11.
Systematic prevalence studies are a fundamental tool for the evaluation of possible interventions. As myopia can affect children and adolescents with incident cases from 6 to 30 years of age, each age group has a specific prevalence. In Bahía Blanca, the “Bahía Ve” (Bahía see) program run by the Secretariat of Health, has been working in this sense since 2008. Visits are scheduled at the city’s educational institutions to carry out ophthalmological check-ups for the early detection of eye diseases in early childhood, with a strong focus on preventive ophthalmology. In the 14 years of the program’s existence, 8,089 children have been screened in public schools. On the other hand, the National University of the South has its own infrastructure linked to the health care of students, where ophthalmological exams are frequently carried out in order to detect alterations but still no data have been published about the prevalence of refractive error in these students. In this context, and given the scarcity of local information on the prevalence of this health condition in university populations, it is essential to generate knowledge in this area. The aim of this study was to show the prevalence of myopia in university students in the city of Bahía Blanca, and to establish whether factors such as outdoor exposure, screen use and reading are related to the occurrence of myopia.
Material and methods
This study was a descriptive cross-sectional study. It included students enrolled in degree courses at the Southern National University in the city of Bahía Blanca who attended the health clinics of the educational institution to undergo a visual acuity test between September and December 2022. In addition to the tests, the students answered a survey in Google forms format where they were asked some questions related to the exposure to the mentioned myopia risk factors. The personal data of each subject was taken into account at the beginning of the research to match each subject with the results given in the survey and follow up tests. These personal data were then removed from the dataset for statistical analysis to ensure the privacy and confidentiality of the results. The questionnaire included an informed consent form, explaining the aims of the research, making it clear that answering the questionnaire was voluntary and anonymous. The study protocol was approved by the Institutional Review Boards, the Teaching Unit of the Provincial’s Health Secretary and the Welfare Secretary of the National University of the South.
The screening consisted of unaided visual acuity testing, performed at the University by the ophthalmologist in charge of the study with a computer visual acuity software at 3 meters distance in a special room under usual artificial lights. The computer software included Snellen letters and tumbling E letters (EChart Acuity, https://echartacuity.com/) which could be changed randomly from subject to subject, allowing that several subjects could be tested simultaneously after explaining the test procedure in groups of 5 children. Those who did not pass the visual acuity test at 20/30 Snellen uncorrected visual acuity test, were sent to the ophthalmological unit with a scheduled visit, given by the ophthalmologist in charge of the program, in order to carry out a complete ophthalmological and subjective and objective refractive testing. When the subjects came for this complete ocular exam the ophthalmologist in charge of the study made a simple subjective test considering previous prescriptions and after this the doctor instilled two drops of cyclopentolate 1% at five-minute intervals, after an initial instillation of one drop of proparacaine 0.05% for topical anesthesia. After one hour, pupil dilation was confirmed and cycloplegic auto-refraction was performed taking the mean of three measurements in each eye (at ±0.25 D) (Topcon RM8000, Tokyo, Japan). The diagnosis was considered to be myopia if the result of the Cycloplegic Spherical Equivalent of the right eye was less than or equal to -0.50D.
The variables collected in the virtual questionnaire were age, gender, career, social security, attendance to support classes outside the University, average hours of daily exposure to open air, screens and reading, visual acuity test results. The variables collected in the subsequent ophthalmological examination were the spherical equivalent, considered as the sum of the value of the spherical component with half the value of the cylindrical component and the family history of high myopia.
Once all data were obtained, they were loaded into an Excel database for further processing. Those few subjects aged 40 years or older and those who did not complete the form because they refused to participate in the research were excluded. In addition, those outlier data where the average hours of exposure of the studied variables exceeded 2 standard deviations were eliminated. The sample needed to obtain representative results was calculated based on data from the University showing a student population of 3,000 new students per year. This resulted in the need for data from 360 students for an expected prevalence of myopia of 20%, considering an error of 5% and a Confidence Interval of 95%.
In first instance, a descriptive analysis was carried out on the total population that attended the visual acuity test using measures of frequency and central tendency. The calculated prevalence was expressed as a percentage with confidence intervals, and the fact that not all students attended the diagnostic cycloplegic test was taken on account estimating that the prevalence would be similar in those cases excluded or included in the cyclo test. In second instance, a logistic regression analysis of myopia as the dependent variable vs. independent environmental factors as average daily hours of outdoor exposure, screens exposure and reading exposure, adjusted by age and gender and tutorials. The results of the ODSS RATIO (OR), its 95% confidence interval and the p-value are described, with a p value of less than 0.05 being considered significant. IBM-SPSS 25.0 software was used for data processing.
Results
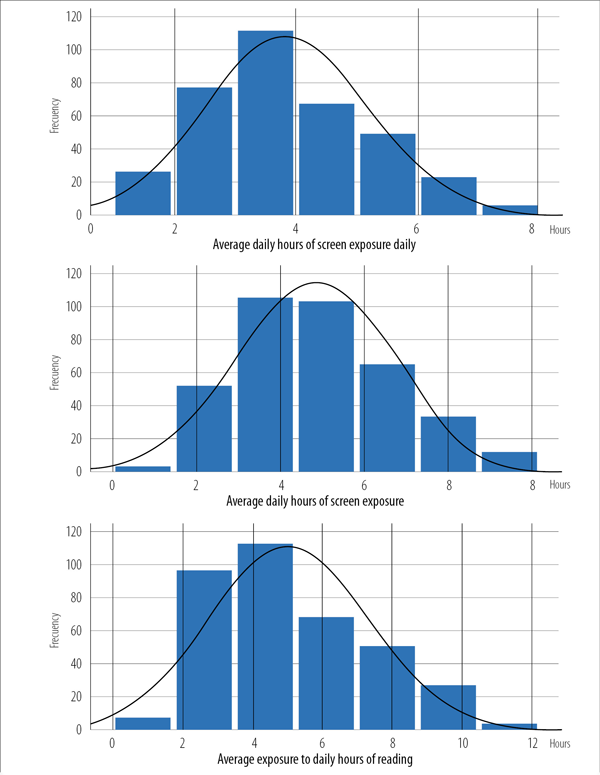
A total of 413 university students aged 18-39 years were studied between September and December 2022. The mean age was 20.78 years, and 67.8% were female (n=280). In the questionnaire, 78% (n=330) reported having social security coverage and 20% (n=82) reported attending tutorial classes outside the university. On the other hand, 84% (n=346) walked or cycled to university, with an average trip time of 46 minutes (Table 1). The average daily outdoors exposure was 3.8 hours, screens were seen for an average of 5 hours/day, and 5.8 hours/day were spent reading (Fig. 1). Out of the total number of students, 33% (n=136) had an impaired visual acuity test, for which they were subsequently called for full refractive examination and diagnosis (Table 1).
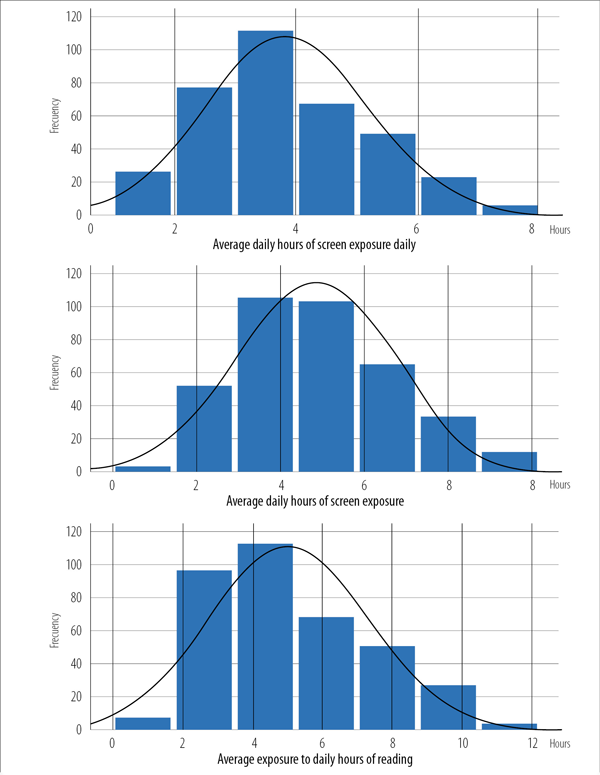
Figure 1. Frequency distribution of main variables.
There were 136 students who did not reach the 20/30 visual acuity threshold, and 84.6% of them (n=115) attended the refractive testing. The cycloplegic examination showed that 82.6% of those (n=95) were diagnosed with myopia. The estimated prevalence of myopia was then 27.2% (95%CI=22.9-31.5%) (including 17 possible myopia subjects among the 21 who failed the refractive testing). The mean outdoor exposure in patients with myopia was 3.73 hs, while those without myopia was 3.85 hs (p=0.07). The mean exposure to screens was 5.09 for those with myopia and 4.75 for those without (p=0.13). Finally, the mean number of hours of daily reading was 5.24 for those with myopia and 4.96 for those without (p=0.13).
Table 1. Main outcome measures of the studied population.
Variables |
Mean |
Median |
Mode |
SD |
Age (years) |
20.78 |
20 |
19 |
3,19 |
Time travelling outdoors to the university (mins) |
46.94 |
40 |
40 |
12.5 |
Total mean daily exposure outdoor (hs) |
3.8 |
3.5 |
3.2 |
1.2 |
Total mean daily exposure to screens (hs) |
5 |
4.7 |
4 |
2.2 |
Total mean daily exposure to reading (hs) |
4.8 |
4.7 |
3.4 |
1.8 |
Having social security coverage n= (%) |
330 (78%) |
83 (22%) |
||
Positively taking tutorial classes n=(%) |
82 (20%) |
331(80%) |
||
Table 2. Logistic regression with the association between myopia and the independent variables. |
|||||||||||
A |
B |
Error |
Wald |
|
Sig. (p) |
OR |
IC95% |
||||
Inferior |
Superior |
||||||||||
|
Age |
.048 |
.037 |
1.678 |
|
.195 |
1.049 |
.976 |
1.127 |
||
Gender |
-.359 |
.297 |
1.465 |
|
.226 |
.698 |
.390 |
1.249 |
|||
Tutorials |
-.898 |
.389 |
5.323 |
|
.021 |
.407 |
.190 |
.874 |
|||
Outdoors |
-.075 |
.101 |
.541 |
|
.462 |
.928 |
.761 |
1.132 |
|||
Reading |
.084 |
.058 |
2.062 |
|
.151 |
1.088 |
.970 |
1.219 |
|||
Screens |
.083 |
.071 |
1.389 |
|
.239 |
1.087 |
.946 |
1.249 |
|||
Constant |
-2.415 |
1.053 |
5.257 |
|
.022 |
.089 |
|
|
|||
|
|||||||||||
A binary logistic regression model was constructed where the dependent variable was the diagnosis of myopia and the independent variables were the 3 exposure factors adjusted for age, gender and attendance to support classes. The results of the Odds ratio with confidence intervals and significance level are shown in Table 2. The model as a whole showed statistical significance (p=0.04) with an R Square of 6%. The OR for outdoor exposure was less than 1, while screens and reading was greater than 1, although the results were not statistically significant. The OR for taking tutorial classes was significantly associated with presence of myopia.
Discussion
The present study reports the prevalence of myopia in subjects at University entrance in the city of Bahia Blanca. The prevalence was relatively low compared to that of Asian Urban environments, where similar aged youngsters have between 70%-90% prevalence of myopia1. But is relatively higher than the prevalence found in a similar urban environment in Argentina in adults aged 40+ where the prevalence was 14%12. Even in the same country, the prevalence in 2005 for a population of office workers with a mean of 6 years of university study was also near 30% like in the entrance to university in the present study13. It is possible that the finding of high amounts of outdoor activities in this population of students (even with high loads of nearwork) drives a relatively low prevalence of myopia in studies of Argentina. Another study with a similar questionnaire showed that children spend 27 hours per week outdoors in Buenos Aries city, one of the most extensive times outdoors reported in the literature14. In this sense the 4 hours of primary and secondary schooling that our country has allows children to spend a lot of time outdoors15. In this sense only the big cities in the country (Buenos Aires, Rosario, Cordoba and Mendoza) have extensive bocks of high-rise buildings where children spend their time indoors in apartments with air conditioned. In 2021, a study was published that assessed the importance of outdoor exposure in university students in Mendoza and the prevalence of myopia16. In Bahia Blanca, the picture is somewhat different. With a population of three hundred thirty three thousand inhabitants the city has a flat architecture with few zones of high rise buildings17. So the students in the present study had high outdoor exposure.
We did not find any significant association of the risk factors assessed in this cross-sectional study between the myopic and the non-myopic groups. It is possible that some subjects in the non-myopic group may be at risk of developing myopia in the future so a prospective study of risk factors may be a better approach. Another important issue about this study is that myopia was not measured in all subjects but a cut point in 20/30 visual acuity was taken as good vision and non-myopia. This approach was based on the Australian study that suggested that for screening for myopia this cut point would be sensitive and effective.
The use of screens has increased considerably in recent decades. People born after 2010 belong to the T generation and know the world around them through digital screens, with behavior conditioned by immediacy, speed and hyper connectivity18. In this decade children and young adults have grown up surrounded by devices such as smartphones, televisions, tablets or computers, which have become a fundamental part of their daily life19-20. Although the average hours spent on screens is high in this study, both local and international studies report higher averages, especially after the pandemic2, 1- 22.
Several studies link the increased progression of myopia to the use of screens23- 24. Greater exposure to computers and screens among university students has been associated with an increase in myopia25. In the present study, although the mean hours of screens was higher in the group that presented myopia, the difference was significant. It is important, as some research indicate, to take into account other issues involved around the digital habits. Many people use them in the dark and at a close distance, and there is a direct relationship between the high use of digital devices and the low outdoor exposure, making it difficult to establish the direct relationship of that risk factor26-27. In this sense, some authors consider that the results between screen time and myopia are inconclusive, requiring more studies with objective measurements of screen time to evaluate the evidence of an association between the two28.
The relationship of myopia with reading hours is also related to close work. In our study, there were increased hours of reading in the myopic group, although the differences were not statistically significant. For centuries it has been debated whether there is an association between near work activities and myopia29. Huang et al. published a systematic review with studies carried out between 1994 and 2014, where they found only 4 longitudinal studies that suggested an association between reading and myopia, while the others found no such association30. One of the reasons for this inconsistency may be the subjectivity of the parameters with which reading is measured. One of the most solid indicators that have been used recently is a distance less than 30 cm as a condition with myopigenic effects6,31. However, these distances were based on questionnaires, as in the case of the present study, and therefore can only provide ambiguous thresholds for the “risk” zone of closework activities. This is why the use of objective instruments should be required to measure the reading distance, such as the device used in an investigation carried out by Wen et al., where they used a portable instrument that can measure and record the working distance and illumination at the eyes, to obtain information about close work and light levels32.
The lack of significant associations between the studied factors, could possibly be due to the fact that some subjects in the group without myopia are at risk of developing myopia in the future, so a prospective study of risk factors may be a better approach. For example, a study carried out in Portugal in a group of university students, where after 12 years of observation they found an almost double increase in the prevalence of myopia caused by incident adult onset33. Another important issue in this study is that myopia was not measured in all subjects, but a cut-off point of 20/30 visual acuity was taken as good vision and not myopia. This approach was based on the Australian study which suggested that this cut-off point would be sensitive and effective for the detection of myopia34-35.
Conclusions
A prevalence of myopia near 28% was found in incoming students at the National University of the South. The average outdoor exposure of this population is high, being higher in those without myopia, although this difference was not significant. The model constructed, although significant, can explain a low percentage of the event (6%), and although outdoor exposure had an Odds Ratio of less than 1 and screens and reading had an Odds Ratio greater than 1, the model was not significant enough to determine whether these life style habits were associated with myopia. Even so, about 1 in 3 young subjects in this environment with high outdoor exposure are myopic and this needs public health interventions.
References
1. Sankaridurg P, Tahhan N, Kandel H et al. IMI Impact of myopia. Invest Ophthalmol Vis Sci 2021; 62: 2.
2. Morgan I, Rose K. How genetic is school myopia? Prog Retin Eye Res 2005; 24: 1-38.
3. Morgan IG, Wu PC, Ostrin LA et al. IMI risk factors for myopia. Invest Ophthalmol Vis Sci 2021; 62: 3.
4. Morgan IG, Wu PC, Ostrin LA et al. IMI report on risk factors for myopia. Invest Ophthalmol Vis Sci 2021; 62: 3.
5. Ip JM, Rose KA, Morgan IG et al. Myopia and the urban environment: findings in a sample of 12-year-old Australian school children. Invest Ophthalmol Vis Sci 2008; 49: 3858-3863.
6. Ip JM, Saw SM, Rose KA et al. Role of near work in myopia: findings in a sample of Australian school children. Invest Ophthalmol Vis Sci 2008; 49: 2903-2910.
7. Wildsoet CF, Chia A, Cho P et al. IMI Interventions Myopia Institute: interventions for controlling myopia onset and progression report. Invest Ophthalmol Vis Sci 2019; 60: M106-M31.
8. Jonas JB, Xu L, Wang YX. The Beijing Eye Study. Acta Ophthalmol 2009; 87: 247-261.
9. Attebo K, Ivers RQ, Mitchell P. Refractive errors in an older population: the Blue Mountains Eye Study. Ophthalmology 1999; 106: 1066-1072.
10. Katz J, Tielsch JM, Sommer A. Prevalence and risk factors for refractive errors in an adult inner city population. Invest Ophthalmol Vis Sci 1997; 38: 334-340.
11. Holden BA, Fricke TR, Wilson DA et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016; 123: 1036-1042.
12. Sánchez VM, Iribarren R, Latino SG et al. Prevalence of refractive errors in Villa Maria, Córdoba, Argentina. Eye Sci 2016; 31: 68-77.
13. Cortinez MF, Chiappe JP, Iribarren R. Prevalence of refractive errors in a population of office-workers in Buenos Aires, Argentina. Ophthalmic Epidemiol 2008; 15: 10-16.
14. Fernández Irigaray L, Balsa A, Armesto A et al. Outdoor exposure in children from Buenos Aires Province, Argentina. Arch Soc Esp Oftalmol (Engl Ed) 2022; 97: 396-401.
15. Lanca C, Szeps A, Iribarren R, Myopia and Schooling Study Group. Role of tutorial classes and full day schooling on self-reported age of myopia onset: findings in a sample of Argentinian adults. J AAPOS 2022; 26: 314 e1-314. e6.
16. Kotlik C, Zaldivar R, Szeps A et al. Myopia and outdoor sports in university students of Mendoza, Argentina. Oftalmol Clin Exp 2021; 14: 96-102.
17. Instituto Nacional de Estadísticas y Censo (INDEC). [Argentine’s poblation census] 2022. Available in: https://censo.gob.ar/index.php/datos_definitivos/
18. Yin S, Kasraian D, van Wesemael P. Children and urban green infrastructure in the digital age: a systematic literature review. Int J Environ Res Public Health 2022; 19: 5906.
19. Hauk L. Use of media by school-aged children and adolescents: a policy statement from the AAP. Am Fam Physician 2017; 96: 56-57.
20. Strasburger VC, American Academy of Pediatrics. Council on Communications and Media. Policy statement: children, adolescents, substance abuse, and the media. Pediatrics 2010; 126: 791-799.
21. Buffone IR, Romano M, Fernández SL et al. Exposición al uso de pantallas en niños de un sector de la ciudad de Bahía Blanca, Buenos Aires. Rev Asoc Med Bahía Blanca 2019; 29: 47-52.
22. Guo YF, Liao MQ, Cai WL et al. Physical activity, screen exposure and sleep among students during the pandemic of COVID-19. Sci Rep 2021; 11: 8529.
23. Saw SM, Chua WH, Hong CY et al. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci 2002; 43: 332-339.
24. Muhamedagic L, Muhamedagic B, Halilovic EA et al. Relation between near work and myopia progression in student population. Mater Sociomed 2014; 26: 100-103.
25. Fernández-Montero A, Olmo-Jiménez JM, Olmo N et al. The impact of computer use in myopia progression: a cohort study in Spain. Prev Med 2015; 71: 67-71.
26. Loman J, Quinn GE, Kamoun L et al. Darkness and near work: myopia and its progression in third-year law students. Ophthalmology 2002; 109: 1032-1038.
27. Alvarez-Peregrina C, Sánchez-Tena MA, Martínez-Pérez C, Villa-Collar C. The relationship between screen and outdoor time with rates of myopia in Spanish children. Front Public Health 2020; 8: 560378.
28. Lanca C, Saw SM. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol Opt 2020; 40: 216-229.
29. Mutti DO, Zadnik K. Has near work's star fallen? Optom Vis Sci 2009; 86: 76-78.
30. Huang HM, Chang DS, Wu PC. The association between near work activities and myopia in children: a systematic review and meta-analysis. PLoS One 2015; 10: e0140419.
31. Quek TP, Chua CG, Chong CS et al. Prevalence of refractive errors in teenage high school students in Singapore. Ophthalmic Physiol Opt 2004; 24: 47-55.
32. Wen L, Cao Y, Cheng Q et al. Objectively measured near work, outdoor exposure and myopia in children. Br J Ophthalmol 2020; 104: 1542-1547.
33. Jorge J, Braga A, Queirós A. Changes in myopia prevalence among first-year university students in 12 years. Optom Vis Sci 2016; 93: 1262-1267.
34. Leone JF, Mitchell P, Morgan IG et al. Use of visual acuity to screen for significant refractive errors in adolescents: is it reliable? Arch Ophthalmol 2010; 128: 894-899.
35. Wang J, Xie H, Morgan I et al. How to conduct school myopia screening: comparison among myopia screening tests and determination of associated cutoffs. Asia Pac J Ophthalmol (Phila) 2022; 11: 12-18.