Figure 1. Diabetic Retinopathy Tele-Screening Program. Annual visits plan for each rural community. H.I.S: Health Information System.
Assessing potential barriers and facilitators in preparation for implementing a diabetic retinopathy tele-screening program in Argentina
Tomás Ortiz Bassoa, Ariel Paladinib
a Hospital Italiano de Buenos Aires, Argentina.
b Dirección de Atención Primaria y Gestión Sanitaria, Ministerio de Salud de La Pampa, Santa Rosa, Argentina.
Received: July 28th, 2020.
Accepted: August 4th, 2020.
Corresponding author
Dr. Tomás Ortiz Basso
Centro Oftalmológico
Escalante 67
Santa Rosa, La Pampa, Argentina
tomasortizbasso@gmail.com
+54 (02954) 423397
Oftalmol Clin Exp (ISSN 1851-2658)
2020; 13(3): 127-134.
Acknowledgments
We acknowledge the support of La Pampa Health Ministry, Ana Lia Fite for her valuable help with the language.
ABSTRACT
Objective: Tele-screening programs against blindness have proved to be effective in many countries. However, there are lots of difficulties that could directly influence their execution, and scaling them up could be a hard challenge. This study aims to identify barriers and facilitators for implementing a DR tele-screening program in a rural area of Argentina.
Methods: A qualitative research study was performed. Unstructured interviews with the healthcare team were made and a Consolidated Framework for Implementation Research to assess details of the program was carried out.
Results: Main enablers are simple examination, good organizational structure, and political decision to implement the program. Principal barriers are work overload, initial high costs, and cultural rejection.
Conclusion: Barriers and facilitators should be assessed before implementing a DR Tele-Screening Program. It is recommended to gain political support and face cultural barriers before the implementation.
Keywords: telemedicine, vision screening, diabetic retinopathy, glaucoma, blindness, Argentina, La Pampa (province).
Evaluando posibles barreras y facilitadores para implementar un programa de tele-screening de retinopatía diabética en la Argentina
RESUMEN
Objetivo: Los programas de tele-screening han demostrado ser eficaces para disminuir la ceguera en muchos países de mundo. Sin embargo, existen muchas dificultades que influyen directamente en su ejecución. El objetivo de este estudio fue identificar barreras y facilitadores para implementar un programa de tele-screening de retinopatía diabética en una zona rural de Argentina.
Métodos: Se realizó un estudio cualitativo a través de entrevistas no estructuradas con el equipo de atención médica de la provincia de La Pampa. Para identificar barreras y facilitadores del programa se conformó un marco consolidado para la investigación de implementación.
Resultados: Los principales facilitadores hallados fueron: contar con un examen de retina simple, tener una estructura de atención médica organizada y buscar la decisión política de implementar el programa. Dentro de las mayores barreras se encuentran: la sobrecarga laboral, los altos costos iniciales y el rechazo cultural hacia la teleoftalmología.
Conclusión: Antes de implementar un programa de tele-screening se deben evaluar los posibles obstáculos y facilitadores que conlleva. Se recomienda obtener apoyo político y hacer frente a las barreras culturales antes de su implementación.
Palabras clave: telemedicina, tamizaje masivo, retinopatía diabética, glaucoma, ceguera, Argentina, La Pampa (provincia).
Avaliando possíveis barreiras e facilitadores para a implementação de um programa de tele-screening de retinopatia diabética na Argentina
RESUMO
Objetivo: Os programas de tele-screening tem demostrado ser eficientes para diminuir a cegueira em muitos países do mundo. Porém, existem muitas dificuldades que influenciam diretamente em sua execução. O objetivo deste estudo foi identificar barreiras e facilitadores para a implementação de um programa de tele-screening de retinopatia diabética em uma zona rural da Argentina.
Métodos: realizou-se um estudo qualitativo através de entrevistas não estruturadas com a equipe de atenção médica da província de La Pampa. Para identificar barreiras e facilitadores do programa se formou um quadro consolidado para a pesquisa de implementação.
Resultados: Os principais facilitadores encontrados foram: contar com um exame de retina simples, ter uma estrutura de atenção médica organizada e buscar a decisão política para a implementação do programa. Dentro das maiores barreiras foram encontradas: a sobrecarga de trabalho, os altos custos iniciais e a rejeição cultural para a teleoftalmologia.
Conclusão: Antes de implementar um programa de tele-screening devem-se avaliar os possíveis obstáculos e facilitadores que implica. Recomenda-se obter apoio político e fazer frente as barreiras culturais antes de sua implementação.
Palavras clave: telemedicina, programas de rastreamento, retinopatia diabética, glaucoma, cegueira, Argentina, La Pampa (província).
INTRODUCTION
Diabetic retinopathy (DR) is the leading cause of blindness in working age people and it is estimated that its prevalence will triplicate by 20501-2. Main cohort studies estimate that 3% to 10% of diabetic patients have vision-threatening DR3. It is known that severely visually impaired people represent high sanitary costs4. If global prevention measures are not taken, society could be hardly stricken either in terms of public health and financial costs5.
Blindness caused by diabetes can be reduced up to a 50% with a proper medical treatment6. To achieve this, an early diagnosis is of vital importance. The American Diabetes Association recommends an annual eye examination, however, only a third of the population adheres to this advice7-8. Poor adherence is associated with lack of information, lack of access or geographical restrictions9.
Currently, in Argentina inequalities in health system access are frequent. Scanty human resources, reduced incomes, long distances, and system centralization are the main causes of this situation.
Within this context, telemedicine stands as a cutting-edge short cut to solve this problem10. It represents an improvement in the access to sanitary system for many patients, mainly elderly people, chronic patients or those detached from health care centers11.
DR tele-screening programs have been developed all around the world12-13. However, although there is enough evidence to support these programs, their outcomes in different contexts are unknown. There are many factors that may influence the effectiveness and accomplishment of scientific innovations in daily practice14. Therefore, in recent years, implementation research studies have been emerging, aiming to characterize and contextualize an intervention, trying to improve the quality and effectiveness in real world14.
The Consolidate Framework for Implementation Research (CFIR) was developed, to understand the reasons why the process may or may not be successful. It is divided into 5 constructs: intervention characteristics, inner setting, outer setting, individual characteristics and process, each of which should be thoroughly evaluated before the implementation of any program15.
The purpose of this study is to describe the use of the CFIR to identify barriers and facilitators for the implementation of a DR tele-screening program in Argentina.
METHODS
Study design
To identify barriers and enablers for the implementation of a DR tele-screening program, we conducted a qualitative study. The CFIR constructs were fulfilled based on personal interviews to ophthalmologists, endocrinologists, primary care practice leadership, clinicians, nurses, informatic and administrative staff.
Unstructured interviews were conducted. They aimed at understanding the perspectives that interviewees had regarding their lives, experiences, or situations. Heads and leaders of each field were selected for the interviews. Interviewees were professionals with more than 10 years of expertise in their fields. Interviews were conducted a year before the implementation began. They were performed in a Health Ministry office and in the hospitals where the interviewees worked. Several face to face interviews were performed. Each one lasted between 1 and 4 hours. The interviewers were the 2 authors of this paper. Main outcomes of each interview were registered. The authors of this paper discussed and analyzed barriers and enablers after each interview.
This study adhered to the tents of the Declaration of Helsinki and Institutional Review Board approval was obtained.
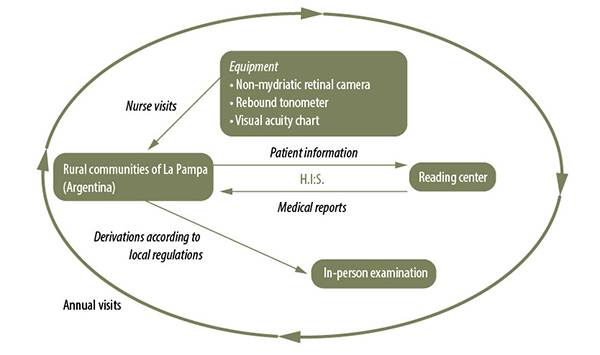
DR tele-screening program (Fig. 1)
The program will take place in rural communities of La Pampa (Argentina) with no ophthalmologist on a permanent basis, so patients need to travel long distances. The program will be equipped with a non-mydriatic retinal camera (Digital Retinography System [DRS], CenterVue SpA, Padova, Italy) to take two images from each eye, a rebound tonometer (Icare ic100, Icare Finland Oy, Vantaa, Finland) and a visual acuity chart. A nurse will be trained to operate this equipment and will have a standardized operating procedures manual.
The population of each community will be identified by the informatic department through the “diabetes diagnosis” in the electronic records. Then, each primary care team will confirm the diagnosis of each patient, before the tele-screening team visits the community.
People in each community will be informed about the program development through phone calls and public announcements. Diabetic patients will be assessed by a nurse in each community health care center. The images will be encrypted and uploaded in the electronic history, ensuring patients’ identities. Images comply with Digital Imaging and Communications on Medicine (DICOM) standards16.
Ophthalmologists will evaluate images from a central reading center and classify them according to the International Clinical Diabetic Retinopathy Study scale17. Medical reports will read as follows: 1) normal, perform an annual examination; 2) mild retinopathy, perform an annual examination; 3) moderate retinopathy, visit an ophthalmologist during the next 6 weeks; 4) severe retinopathy, visit an ophthalmologist during the next 7 days. Patients who need an ophthalmologist appointment will be transferred to the central hospital. The health system will oversee patients’ derivations according to local regulations.
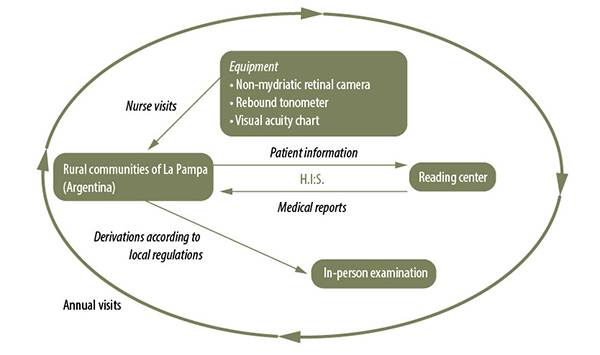
Figure 1. Diabetic Retinopathy Tele-Screening Program. Annual visits plan for each rural community. H.I.S: Health Information System.
Outcomes definitions
A description of the 5 constructs of the CFIR was performed: 1) intervention characteristics: refers to the particular characteristics that would made the program successful, including evidence strength, relative advantage, adaptability, trialability, complexity, cost; 2) inner setting: describes the possible interaction between internal components of the program, including structural characteristics, networks, culture, implementation climate; 3) outer setting: possible interactions between external factors and the program, including patients’ needs and resource, peer pressure, external policies; 4) individual characteristics: analyzes the possible actions and behaviors of the participating individuals, including knowledge and beliefs about the intervention; 5) process: actions and activities that should take place to have an effective program, including planning, executing and evaluating18.
Data were compiled, and descriptive statistics were calculated by using Microsoft Excel for Office 365 (Microsoft Corporation, Redmond, WA).
RESULTS
Consolidated Framework for Implementation Research (Fig. 2)
Intervention characteristics
Reviewing the literature, similar programs have been found, implemented all around the world, and some of them have proved to be cost-effective19. Alternative solutions were evaluated, such as an ophthalmologist travelling around the different communities. This will result in higher costs and will be significantly stressful and more time demanding.
This program is the simplest way to tackle the proposed problem, a diabetic patient undergoes a quick eye examination without pupil mydriasis in his own town, and in one week’s time he receives the report. Through image digitization, sub-processes reduction and continuous audits, complexity threats that may lead to loss reports or data misinterpretation, would be avoided.
The program will have core components such as a protocol, a schedule of visits and audits. The program aims at adapting to the needs and environment of each community. This “adaptable periphery” becomes more versatile depending on the members of each team and on each team’s cycle (members on holidays, local epidemics, economy, or politics).
The program has been tested in Rancul, a rural town where the population showed great interest in the proposal. During two visits, 58 type 1 and 2 diabetic mellitus people were checked. In this pilot test, 61.5% of the population had had a previous fundus examination performed, and only 15.3% had had it assessed in the past year. DR was found in 38.4% of the patients. This test allowed researchers to assess and improve the implementation logistics, analyze possible problems and to strategically anticipate contingencies.
Even though equipment acquisition may represent a barrier at the beginning, in the end it would be cost-effective, as only 10% to 30% of participants would undergo a second assessment20. The costs of complementary studies and treatments for people without medical insurance will be covered by the Government.
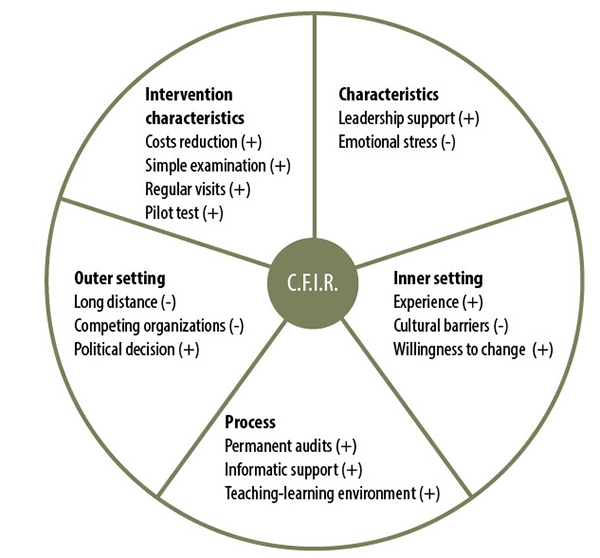
Figure 2. Main enablers and barriers of the Program, according with the CFIR constructs. CFIR: Consolidated Framework for Implementation Research; (+) enabler; (-) barrier.
Outer setting
Rural populations must travel long distances to access an eye examination. At present, some ophthalmologists go around the province. However, they do not reach all the communities and do not do it regularly, this generally results in late treatments. This program will allow early diagnosis, avoiding time loss and increasing effectiveness.
As many ophthalmologists could feel threatened by the program, meetings were organized to explain that the program gives relevance, hierarchy and organizes appointment management. Thus, ophthalmologists will participate and work for the program as part of the solution.
Political will to implement the program is the main facilitator, so guidelines should aim at keeping it active in time. Complementary studies and treatments, the journeys, and the lodging, will conform to present requirements of the system.
Inner setting
La Pampa Health Ministry has experience with a similar program, that takes a mammograph to different communities. This experience has helped healthcare teams develop a scaffold of working methodology.
Rural communities share a solidary fellowship culture, within which everyone tries to collaborate with each other. Healthcare centers are settled within small rural communities and the heath staff is clearly aware of the populations needs. They complain about the lack of eye doctors’ visits along the year.
Endocrinologists, who receive patients from these towns, also complain about the lack of possibilities for their patients to have an eye examination regularly. Besides, those who finally have access to it, rarely return with the results.
Characteristics of individuals
New procedures sometimes result in doubts, mistakes, and loss of time, that may lead to emotional exhaustion within the teamwork. The strategy is to make everyone feel as key participants of the program, so they will be more motivated and will strive to adapt to it. Group support is essential during this stage. Social events among teams should be organized to construct knowledge, to foster brainstorming and peer acknowledgement.
Feedback and achievement recognition will be forwarded with an analysis of the situation in each community.
Process
All the communities of the area will be visited during the first year and previous meetings should be held with each team to reach consensus about needs. Each teamwork will be trained according to the diabetic patient’s healthcare recommendations and on the program methodology. Trainings will include presential interactive instruction and e-learning tools management. A continuous teaching-learning environment will we carried out in all the implementing process.
Meanwhile, diabetic patients and their relatives, will be contacted and informed about the importance of a regular health check-up to prevent further complications.
The program will use the informatic system to have quick access to all information related to the intervention. Audits will be carried out for patient’s follow-up, to foster feedback to teamwork and to improve the quality of the program.
DISCUSSION
One of the main facilitators for implementing a RD tele-screening program was the government´s support. Other programs have proved that without federal appropriations or research grants, the sustainability and the scaling-up, were not possible21. So, having the government support from the start is the key piece to put it into practice.
It is vital that all the stakeholders of the program recognize the advantages of its implementation. If they perceive the benefit it will be surely successful22. Stakeholders, admitted that by applying this technology they will improve patient’s quality of life, decrease the risk of blindness and save economic resources.
A program must have a core component and an adaptable periphery. The more flexible the intervention is, the more effective the program will be22. The proposed program has a central component that stakeholders must follow, but it will be adapted to the local conditions. Flexibility is the key for a successful program implementation.
A pilot test was performed in a small community, which has a strong positive association with effective implementation. It is highly recommended to test the intervention in small scale first, in order to adjust details before going on22.
Understanding population needs is one of the main issues, since programs which focus on population requirements are more likely to be successful23. Primary healthcare staff are aware about the imperative need of an ophthalmologist for their community, and this program fulfills this need.
It is important to evaluate competing organization before implementing a program22. In a highly competitive market, peers could feel threatened by the program and may boycott it. It is important to make them understand that the program, far for threatening their practice is directed to enhance primary health care and secondary prevention actions. This will foster the relationship between care levels, improving the quality of health service24.
Culture also influences the program dynamics and stands as one of the most critical barriers. Introducing a cultural-sensitive model would improve the program integration25. This program will take advantage of the cultural setting, as health teams are part of the community, more commitment and a strong emotional component will be added.
It is important to identify the implementation climate, in order to evaluate the attitude towards change and the receptivity for change in working habits. The primary care team of each community involved in our program is open for innovation because they understand that these initiatives will favor the population’s welfare. It is of great importance to achieve empathy among team members so they can adapt easily and give priority to the model. Setting a learning friendly environment, with constant feedback, is essential to maintain motivation over time.
Careful planning is basic for effective implementation. So, a one-year program schedule was stablished, and training activities were organized for the staff before the start. Quality of execution should be measure all through the program. In this way we enforce the program sustainability.
One limitation of our study is that we did not interviewed people from the rural community. However, we interviewed health care professionals, who indirectly gave us information about the rural community´s needs. Another is that interviews were not recorded, and a detail presentation could not be done, however the information was registered and taken into account in the program design.
CONCLUSION
This study proved that one of the main enablers for the implementation of a DR tele-screening program is government´s support, and that the principal barriers to overcome are the cultural interactions. Foundations to scale-up to other similar regions and to implement similar programs were settled down.
REFERENCES
1. International Diabetes Federation. IDF Diabetes atlas. 9th ed. Brussels: IDF, 2019. Available in: https://www.diabetesatlas.org [cited: July 2020].
2. Kempen JH, O’Colmain BJ, Leske MC et al. The prevalence of diabetic retinopathy among adults in the United States. Arch Ophthalmol 2004; 122: 552-563.
3. Saaddine JB, Honeycutt AA, Narayan KMV et al. Projection of diabetic retinopathy and other major eye diseases among people with diabetes mellitus: United States, 2005-2050. Arch Ophthalmol 2008; 126: 1740-1747.
4. Romero-Aroca P, de la Riva-Fernandez S, Valls-Mateu A et al. Cost of diabetic retinopathy and macular oedema in a population, an eight year follow up. BMC Ophthalmol 2016; 16: 136.
5. Panton UH, Bagger M, Barquera S. Projected diabetes prevalence and related costs in three North American urban centres (2015-2040). Public Health 2018; 157: 43-49.
6. Ferris FL 3rd. How effective are treatments for diabetic retinopathy? JAMA 1993; 269: 1290-1291.
7. Fong DS, Aiello L, Gardner TW et al. Diabetic retinopathy. Diabetes Care 2003; 26 (Sup 1): S99-S102.
8. Sloan FA, Yashkin AP, Chen Y. Gaps in receipt of regular eye examinations among medicare beneficiaries diagnosed with diabetes or chronic eye diseases. Ophthalmology 2014; 121: 2452-2460.
9. Moss SE, Klein R, Klein BEK. Factors associated with having eye examinations in persons with diabetes. Arch Fam Med 1995; 4: 529-534.
10. Rathi S, Tsui E, Mehta N et al. The current state of teleophthalmology in the United States. Ophthalmology 2017; 124: 1729-1734.
11. Rodríguez Cabrera K, Vélez Ospina JA. Impacto de las TIC en el nivel de innovación en América Latina y el Caribe: estimaciones econométricas a nivel de un panel. Redes.com: revista de estudios para el desarrollo social de la comunicación 2014; 9: 341-360.
12. Kirkizlar E, Serban N, Sisson JA et al. Evaluation of telemedicine for screening of diabetic retinopathy in the Veterans Health Administration. Ophthalmology 2013; 120: 2604-2610.
13. Zanotto BS, Etges APB da S, Siqueira AC et al. Avaliação econômica de um serviço de telemedicina para ampliação da atenção primária à saúde no Rio Grande do Sul: o microcusteio do projeto TeleOftalmo. Cien Saude Colet 2020; 25: 1349-1360.
14. Suárez-Obando F, Gómez-Restrepo C, Castro-Díaz SM. Ciencias de la implementación: de la evidencia a la práctica. Acta Med Colomb 2018; 43: 207-216.
15. Kirk MA, Kelley C, Yankey N et al. A systematic review of the use of the Consolidated Framework for Implementation Research. Implement Sci 2016; 11: 72.
16. Digital Imaging and Communications in Medicine (DICOM). Arlington, VA: DICOM Secreariat, Available in: https://www.dicomstandard.org/
17. Wilkinson CP, Ferris FL 3rd, Klein RE et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 2003; 110: 1677-1182.
18. The Consolidated Framework for Implementation Research [en línea]. Ann Arbor, MI: CFIR Research Team-Center for Clinical Management Research. Available in: https://cfirguide.org/ [cited: July 2020].
19. Sharafeldin N, Kawaguchi A, Sundaram A et al. Review of economic evaluations of teleophthalmology as a screening strategy for chronic eye disease in adults. Br J Ophthalmol 2018; 102: 1485.1491.
20. Andonegui J, Serrano L, Eguzkiza A et al. Diabetic retinopathy screening using tele-ophthalmology in a primary care setting. J Telemed Telecare 2010; 16: 429-432.
21. Liu Y, Torres Diaz A, Benkert R. Scaling up teleophthalmology for diabetic eye screening: opportunities for widespread implementation in the USA. Curr Diab Rep 2019; 19: 74.
22. Greenhalgh T, Robert G, Macfarlane F et al. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q 2004; 82: 581-629.
23. Shortell SM, Marsteller JA, Lin M et al. The role of perceived team effectiveness in improving chronic illness care. Med Care 2004; 42: 1040-1048.
24. Rodríguez Villa S, Alonso Álvarez C, de Dios Del Valle R et al. Análisis de un programa de teleoftalmología para el cribado de retinopatía diabética en área rural tras cinco años. Arch Soc Esp Oftalmol 2016; 91: 426-430.
25. Gershon RRM, Stone PW, Bakken S, Larson E. Measurement of organizational culture and climate in healthcare. J Nurs Adm 2004; 34: 33-40.