
SURGICAL TECHNIQUES AND DIAGNOSTIC PROCEDURES
Modified partial bisection surgical technique for the extraction of the dislocated intraocular lens-capsular bag complex: novel adaptation in a case of dead bag syndrome
Andrés Germán Alza
Clínica Privada de Ojos Dr. Enrique Alza, La Plata, Argentina.
Corresponsal author
Dr. Andrés Germán Alza
Clínica Privada de Ojos Dr. Enrique Alza
Calle 12, nro. 662
(1900) La Plata, provincia de Buenos Aires
Argentina
+ 54 9 221 4219682
andresalza@hotmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2023; 16(4): e442-e451.
Abstract
A modification of the surgical technique, called partial bisection, is presented for the extraction of a dislocated three-piece hydrophilic acrylic monobloc folding intraocular lens-capsular bag complex. The novel surgical technique uses pre-existing incisions that were made during cataract surgery. It consists of trapping the haptic of the IOL in the second-hand corneal incision to perform a partial cut of the optics of the intraocular lens. The technique was performed in an adult patient with dead bag syndrome, and no subsequent complications were observed. It is concluded that the modified partial bisection technique is safe, effective, and less likely to cause complications leading to pars plana vitrectomy.
Keywords: intraocular lens implantation, surgical technique, modified partial bisection, dead bag syndrome.
Técnica de bisección parcial modificada para la extracción del complejo de lente intraocular-bolsa capsular dislocada: adaptación novedosa para un caso de síndrome de bolsa muerta
Resumen
Se presenta una modificación en la técnica quirúrgica denominada bisección parcial para la extracción del complejo lente intraocular plegable de acrílico hidrofílico monopieza de tres hápticas-saco capsular luxado. La novedosa técnica utiliza las incisiones preexistentes que se realizaron durante la cirugía de la catarata. Implica atrapar el háptico de la lente intraocular en la incisión corneal de la segunda mano para realizar el corte parcial de la óptica de la lente. Se realizó en un paciente adulto con síndrome de la bolsa muerta y no se observaron complicaciones posteriores. Se concluye que la técnica es segura, efectiva y menos probable que cause complicaciones que conduzcan a una vitrectomía pars plana.
Palabras clave: implante de lente intraocular, técnica quirúrgica, bisección parcial modificada, síndrome de la bolsa muerta.
Técnica de bissecção parcial modificada para remoção do complexo lente intraocular-saco capsular luxado: nova adaptação para um caso de síndrome do saco morto
Resumo
Uma modificação na técnica cirúrgica chamada bissecção parcial é apresentada para a extração do complexo saco capsular deslocado da lente intraocular dobrável, complexo, de três hápticos, de peça única, em acrílico hidrofílico. A nova técnica utiliza incisões pré-existentes que foram feitas durante a cirurgia de catarata. Envolve prender a alça da lente intraocular na incisão corneana da segunda mão para realizar o corte parcial da óptica da lente. Foi realizado em paciente adulto com síndrome do saco morto e não foram observadas complicações subsequentes. Conclui-se que a técnica é segura, eficaz e com menor probabilidade de causar complicações que levem à vitrectomia via pars plana.
Palavras-chave: implante de lente intraocular, técnica cirúrgica, bissecção parcial modificada, síndrome da bolsa morta.
Introduction
The causeless dislocation of the intraocular lens-capsular bag complex (IOLCBC) years after implantation is a rare late complication called “dead bag syndrome” (DBS). It occurs when a transparent capsule weakens, divides, and/or dislocates without a causal agent and spontaneously. The aim of this work is to present a surgical technique for the extraction of the IOLCBC, without a defined support, by entrapping the haptic in the second-hand corneal incision and its subsequent extraction by the modified partial bisection technique. The technique offers greater safety at the time of explantation by providing support, preserving tissue integrity and taking advantage of pre-existing incisions as a result of previous surgeries.
Case
We present the case of a 75-year-old adult male with a history of high myopia and myopic maculopathy in his left eye. In 2008, he underwent bilateral cataract surgery without complications with the implantation of a three-haptic Stabibag hydrophilic monopiece acrylic lens foldable from the IOL Tech company (Fig. 1). In 2011, the treatment was completed with a Nd:YAG laser capsulotomy in both eyes. After several years of ophthalmological controls, the IOLCBC remained intact, the intraocular lens (IOL) was centered and there was no history of pseudophacodonesis.In March 2023, the patient returned to the emergency room, reporting a decrease in vision and sudden monocular diplopia affecting his left eye. He denied any history of previous eye trauma prior to the consultation. Upon examination with the slit lamp, a dislocation of the intraocular lens-capsular bag complex into the vitreous cavity was observed (Fig. 2). Given the findings described above, it was decided to perform complementary studies for a more detailed evaluation. Digital retroillumination with Scheimpflug camera shows a clean posterior crystalline capsule with a long-term posterior capsulotomy (Figs. 3a-b). The study of the anterior segment using a Scheimpflug camera (Fig. 4) and optical coherence tomography (Fig. 5) revealed a dislocated IOLCBC. As a treatment, it was decided to perform a surgical technique for the extraction of the IOLCBC, by trapping one of its haptics in the secondary corneal incision under the partial bisection technique, working only through the anterior segment. Due to his history of high myopia, he did not require a secondary implant. His vision recovered to 20/50, leaving a residual refractive defect of sphere +0.75 and cylinder -1.25 at 105 degrees (Fig. 6), thus considering it a surgical success.

Figure 1. Three-haptic hydrophilic acrylic monopiece implant foldable (Stabibag, from IOL Tech).
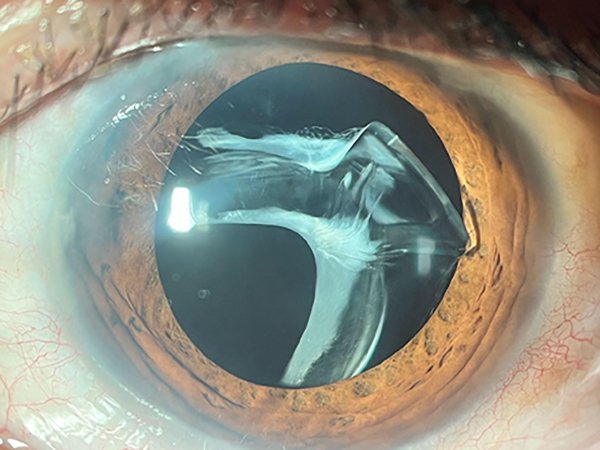
Figure 2. A slit-lamp examination revealed a dislocation of the IOLBC into the vitreous cavity with a clean posterior crystalline capsule with a long-term Nd:YAG capsulotomy.

Figure 3a. Digital retroillumination with Scheimpflug camera showing a clean posterior crystalline capsule with a long-term Nd:YAG capsulotomy.
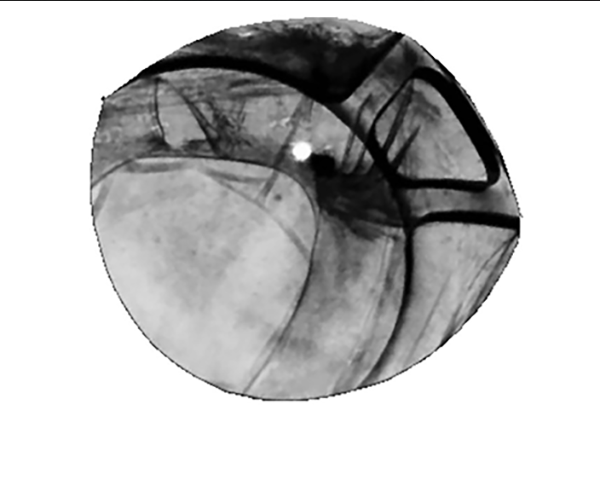
Figure 3b. Digital retroillumination with Scheimpflug camera showing a clean posterior crystalline capsule with a long-term Nd:YAG capsulotomy.

Figure 4. Anterior segment study using a Scheimpflug camera showing a dislocated intraocular lens-capsular bag complex.
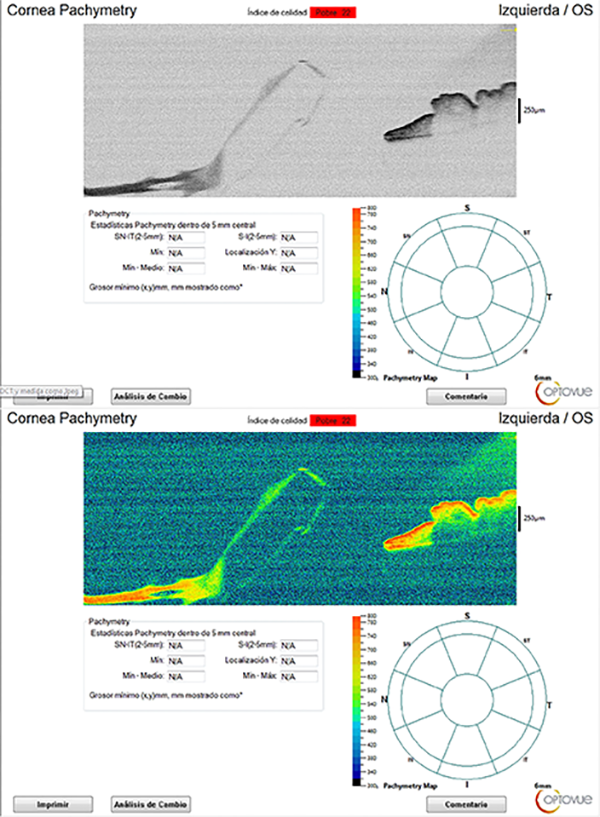
Figure 5. Anterior segment optical coherence tomography showing a dislocated intraocular lens-capsular bag complex.
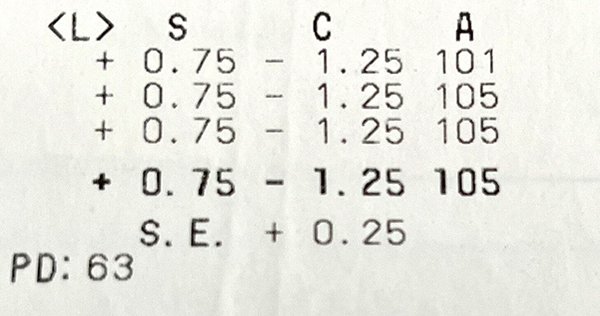
Figure 6. Residual refractive defect of sphere +0.75 and cylinder -1.25 at 105 degrees.
Surgical technique
Before the procedure, the patient was asked to apply one drop of 5% phenylephrine combined with 0.5% tropicamide every 15 minutes for the previous two hours in the conjunctival cul-de-sac.
Once the patient was under the microscope, sub-Tenonian anesthesia was applied with a 19G Stevens curved cannula loaded with a mixture of 0.75 ml of 1% lidocaine and 0.75 ml of 0.5% bupivacaine, both without preservatives.
Surgery was then started using the two incisions, primary and secondary, that had been created previously during cataract surgery in 2008.
The main incision was rescued with a 2.8 mm angled slit knife (Fig. 7).
The secondary incision was rescued first made with a 25 mm 23G blue needle, which was then enlarged with a 15° puncture knife (Fig. 8).
To form the anterior chamber, 3% sodium hyaluronate was added, avoiding pushing the complex but sufficient to protect the corneal endothelium (Fig. 9).
Then, through the second hand incision, a 23G micro holding forceps was introduced to capture the IOLCBC assisted by a 25 mm (1 inch) 23G blue needle previously inserted 4 mm from the sclerocorneal limbus to push the complex upwards and left due to the great displacement of the central pupillary axis (Fig. 10).
Once captured with the micro holding forceps, the left haptic was entrapped in the incision of the second hand, while the optic and the other haptic were dislocated above the iris (Fig. 11).
Using a 25G spatulate cannula, 0.1 mL of 0.01% carbachol intraocular solution was injected behind the complex and a sufficient air bubble to provide further momentary support and stability until the miotic effect takes effect (Fig. 12).
Inserting the full 5.5 mm angled implant knife (for foldable IOLs), the main incision was extended a little further (Fig. 13) and a 5 mm curved Vannas scissors was inserted and cut the implant foldable using the partial bisection technique up to 2/3 of the optic (Fig. 14).
I decided to remove the IOLCBC with Troutman superior rectus forceps —1 x 2 teeth— angled (Fig. 15).
Then, an anterior vitrectomy was performed with a vitrectome and a peripheral iridectomy (Fig. 16).
Finally, the filling of the anterior chamber with air, hydration of the incision, and suturing of the surgical wound with nylon 9 was completed (Fig. 17).
The patient was controlled at 24 hours (Fig. 18) and at 7 days (Fig. 19), who presented a successful recovery.
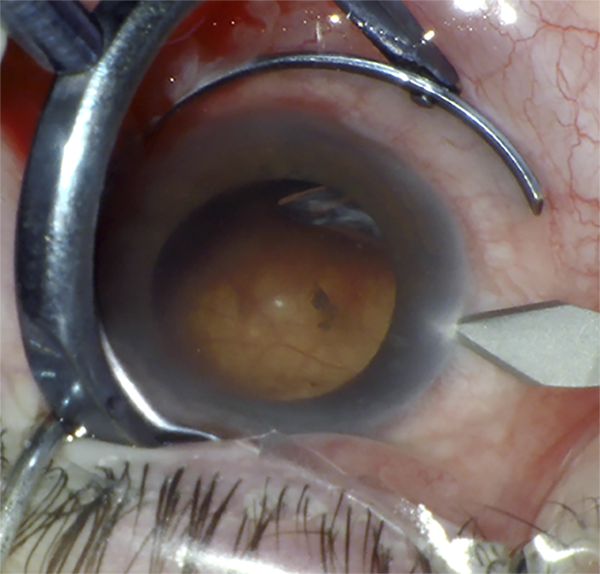
Figure 7. The main incision was rescued with a 2.8 mm angled slit knife.
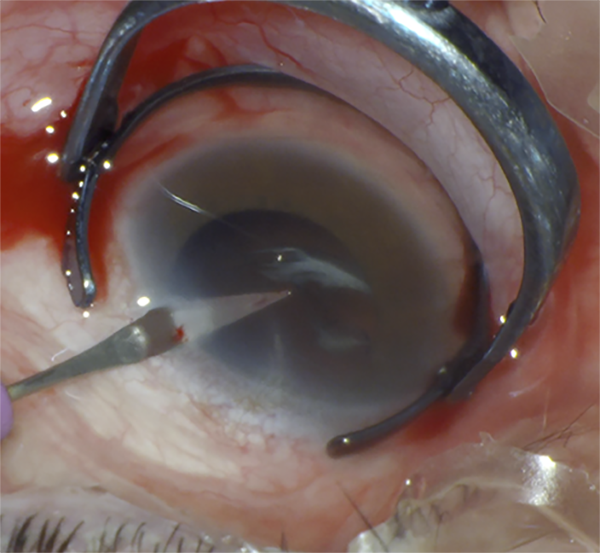
Figure 8. The secondary incision was rescued first made with a 25 mm 23G blue needle, which was then enlarged with a 15° puncture knife.

Figure 9. To form the anterior chamber, 3% sodium hyaluronate was added, avoiding pushing the complex but sufficient to protect the corneal endothelium.
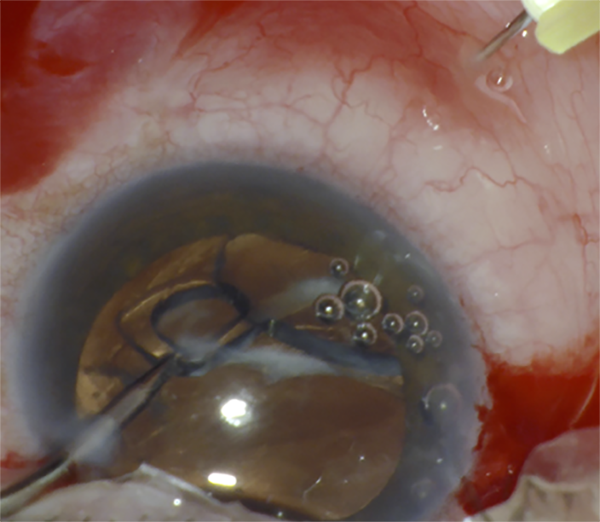
Figure 10. Then, through the second hand incision, a 23G micro holding forceps was introduced to capture the IOLCBC assisted by a 25 mm (1 inch) 23G blue needle previously inserted 4 mm from the sclerocorneal limbus to push the complex upwards and left due to the great displacement of the central pupillary axis.
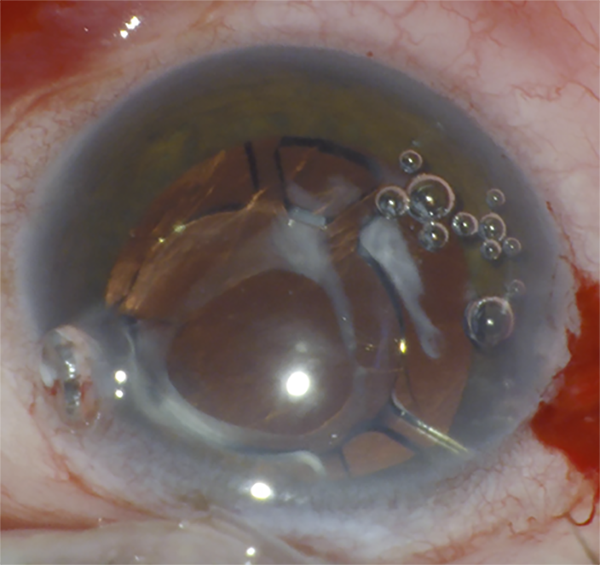
Figure 11. Once captured with the micro holding forceps, the left haptic was entrapped in the incision of the second hand, while the optic and the other haptic were dislocated above the iris.
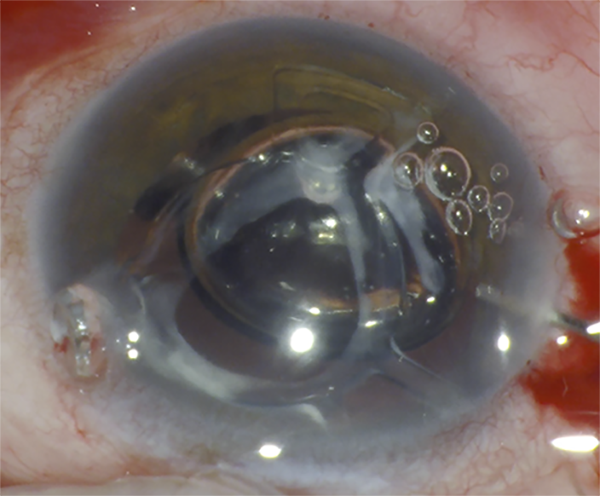
Figure 12. Using a 25G spatulate cannula, 0.1 mL of 0.01% carbachol intraocular solution was injected behind the complex and a sufficient air bubble to provide further momentary support and stability until the miotic effect takes effect.
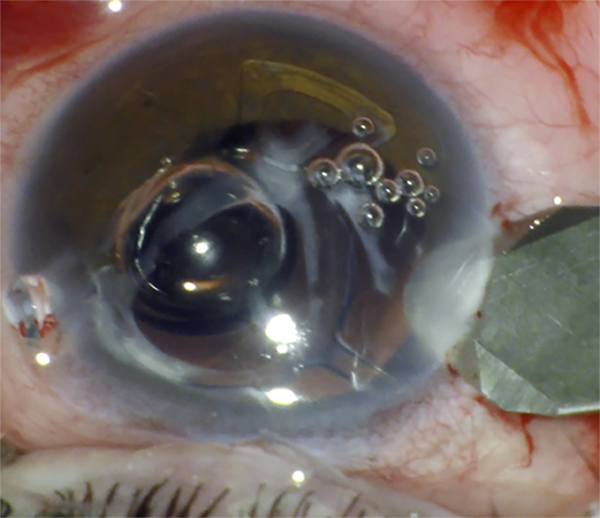
Figure 13. Inserting the full 5.5 mm angled implant knife (for foldable IOLs), the main incision was extended a little further.
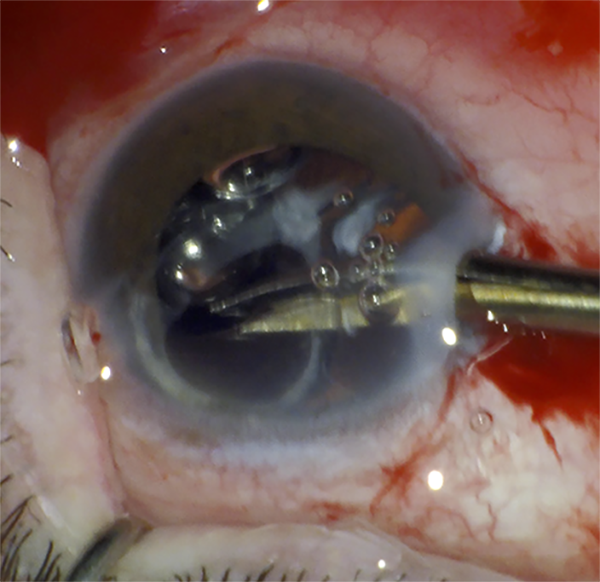
Figure 14. A 5 mm curved Vannas scissors was inserted and cut the implant foldable using the partial bisection technique up to 2/3 of the optic.

Figure 15. I decided to remove the IOLCBC with Troutman superior rectus forceps —1 x 2 teeth— angled.

Figure 16. Then, an anterior vitrectomy was performed with a vitrectome and a peripheral iridectomy.
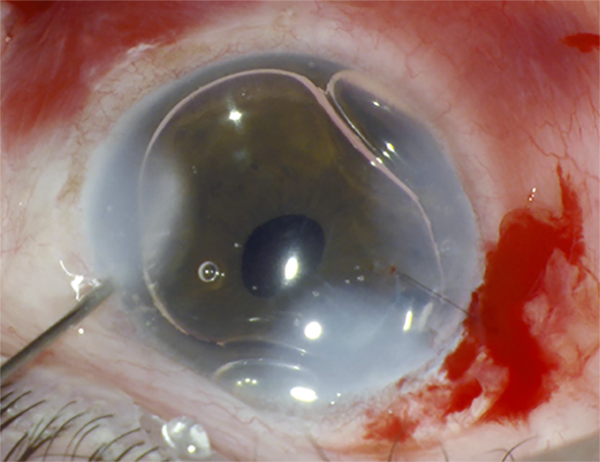
Figure 17. Finally, the filling of the anterior chamber with air, hydration of the incision, and suturing of the surgical wound with nylon 9 was completed.
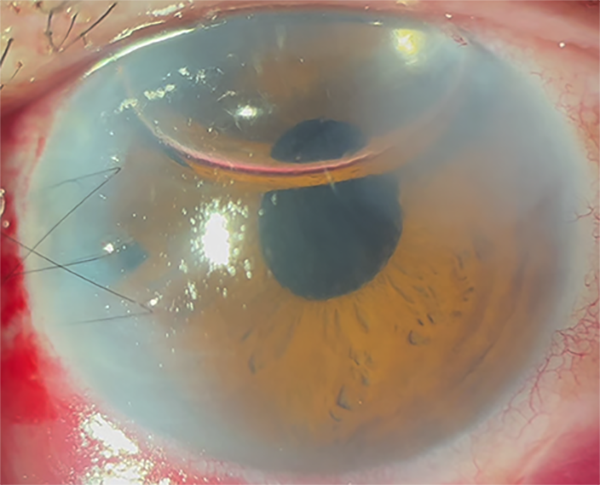
Figure 18. Post-surgical control at 24 hours.

Figure 19. Control at 7 days after surgery.
Discussion
The dislocation of the IOLCBC years after surgery and without apparent cause is a rare late complication initially described by Sam Masket as dead bag syndrome (DBS). Due to its novelty, the exact cause is unknown to date, but it is hypothesized that late postoperative zonular failure would be related to the division and/or delamination of the capsule that occurs at the level of the zonular insertions1-2 and through a different mechanism than pseudoexfoliation. Given the characteristics of the damage, the best option would be to remove all of the IOLCBC, perform an anterior vitrectomy, and then implant, or not, a new IOL. There are several explantation techniques, such as the review by Roberto Fernández Buenaga and Jorge Alió3, which can be divided into 4 different groups:
Complete removal of the intraocular lens through large incisions for the rigid type of lens.
The partial or total cutting of intraocular lenses for folding lenses and smaller incisions, such as cutting in two parts, three parts or simply performing a partial bisection.
Cut the haptic of the intraocular lens, removing only the optic, in the event that removing the haptics puts the integrity of the capsular support at risk.
Intraocular lens retraction and removal through even smaller incisions, but with greater risk to surrounding intraocular tissues.
In this case, we chose the intraocular lens partial cut technique, for folding lenses and smaller incisions. We performed a partial bisection similar to the technique described by Jodhbir Mehta et al.4, but we modified the process and adapted the idea of entrapping the haptic of the three-haptic hydrophilic monopiece acrylic intraocular lens foldable in the second-hand corneal incision. This was done because there was no secure support that would prevent the dislocation of the IOLCBC to the fundus during the surgical procedure, which would inevitably lead to a second surgery of vitrectomy for pars plana. Thanks to the novel technique, we were able to explant a one-piece hydrophilic flexible intraocular lens with three haptics without compromising the integrity of the original wound, the iris, the posterior lens capsule, or the corneal endothelium.
Conclusion
The extraction of the IOLCBC, by means of a novel adaptation in the technique of partial bisection modified of entrapping the haptic corresponding to the second hand in a case of DBS, gives the surgeon greater security during the procedure, does not induce damage to surrounding tissues, takes advantage of existing incisions without increasing the risk of astigmatism, and is also easy to reproduce. It is hoped that in the future there will be a series of more cases with a longer follow-up time to evaluate the technique.
References