
ORIGINAL ARTICLES
Axial length changes with diffusion optics multiple segments (DOMS) spectacles for myopia control
Abel Szepsa, Martín De Tomasb, Calos Kotlikc, Rafael Iribarrend
a Ophthalmological Center, Buenos Aires, Argentina.
b International Optical & Ophthalmology, Buenos Aires, Argentina.
c Servicio de Oftalmología, Hospital Notti, Mendoza, Argentina.
d Drs. Iribarren Eye Consultants, Buenos Aires, Argentina.
Received: January 10th, 2023.
Aproved: April 12nd, 2023.
Corresponsal author
Dr. Abel J. Szeps
Gavilán 4103
(1419) Buenos Aires, Argentina
+54 911 5120-6006
abelszeps@gmail.comabelszeps@gmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2023; 16(2): e148-e154.
Funding
Nothing to declare.
Disclosures
The authors declare no conflicts of interest.
Data availability
Data generated in this study are available at reasonable request.
Abstract
Purpose: To evaluate short time axial length changes after the use of an especially designed spectacle with peripheral contrast reduction.
Methods: A pilot study was performed in subjects were tested when using especial peripheral contrast modulation spectacles with a central zone with the distance myopic correction. During the experiment subjects read a book with black letters on white background on a desktop computer with the same brightness in two periods, one with usual spectacles and the second with the especial ones. Before and after these periods, 10 measurements of the axial length of the right eye were made with Lenstar 900 biometer and were averaged up to three decimals.
Results: Eight subjects, whose a mean age was 22.3 ± 5.5 years participated in this study. The mean spherical equivalent of their right eye was -2.31 ± 1.06 diopters. There was a significant difference of +16.1 microns increased axial length from baseline when reading with the usual prescription during the first 40 min period. When subjects read in the same situation with the contrast modulation spectacle, the axial length change significantly reversed, shortening by -9.2 microns (p<0.001 and p=0.002, respectively Student’s t test).
Conclusion: The decrease in axial length with the tested spectacles may be due to choroidal thickening. As myopia development is arrested when choroid becomes thicker, these spectacles could be tested for myopia control in a clinical trial.
Key words: myopia, DOT and DOMS technology spectacles.
Cambios en la longitud axial con anteojos de difusión óptica de múltiples segmentos (DOMS) para el control de la miopía
Resumen
Objetivo: Evaluar los cambios de la longitud axial a corto plazo tras el uso de un anteojo especialmente diseñado con reducción del contraste periférico.
Métodos: Se realizó un estudio piloto en el que se evaluó a sujetos que utilizaban anteojos especiales con modulación del contraste periférico y una zona central con corrección de la miopía lejana. Durante el experimento los sujetos leyeron un libro con letras negras sobre fondo blanco en la computadora con la misma luminosidad en dos períodos: uno con los anteojos habituales y el segundo con los especiales. Antes y después de estos períodos se realizaron 10 mediciones de la longitud axial del ojo derecho con el biómetro Lenstar 900 y se promediaron hasta tres decimales.
Resultados: Ocho sujetos, cuya edad media era de 22,3 ± 5,5 años, participaron en este estudio. El equivalente esférico medio de su ojo derecho era de -2,31 ± 1,06 dioptrías. Se observó una diferencia significativa de +16,1 micras de aumento de la longitud axial con respecto del valor basal al leer con la graduación habitual durante el primer período de 40 minutos. Cuando los sujetos leyeron en la misma situación con el anteojo de modulación del contraste, el cambio de longitud axial se invirtió significativamente, acortándose en -9,2 micras (p<0,001 y p=0,002, respectivamente prueba t de Student).
Conclusiones: La disminución de la longitud axial con los anteojos probados en este estudio puede deberse al engrosamiento de la coroides. Dado que el desarrollo de la miopía se detiene cuando la coroides se engrosa, estos anteojos podrían probarse para el control de la miopía en un ensayo clínico.
Palabras clave: miopía, tecnología, anteojos DOT y DOMS.
Mudanças de comprimento axial com lentes de múltiplos segmentos de difusão (DOMS) para controle de miopia
Resumo
Objetivo: Avaliar as mudanças no comprimento axial a curto prazo após o uso de óculos especialmente projetado com redução de contraste periférico.
Métodos: Foi realizado um estudo piloto no qual foram avaliados indivíduos usuários de óculos especiais com modulação de contraste periférico e zona central com correção de miopia distante. Durante o experimento os sujeitos leram um livro com letras pretas sobre fundo branco no computador com a mesma luz em dois períodos: um com os óculos usuais e o segundo com os especiais. Antes e depois desses períodos, foram feitas 10 medições do comprimento axial do olho direito com o biômetro Lenstar 900 e calculada a média com três casas decimais.
Resultados: Oito sujeitos, com idade média de 22,3 ± 5,5 anos, participaram deste estudo. O equivalente esférico médio de seu olho direito foi de -2,31 ± 1,06 dioptrias. Uma diferença significativa de +16,1 mícrons de aumento do comprimento axial da linha de base foi observada ao ler com a graduação usual durante o primeiro período de 40 minutos. Quando os sujeitos leram na mesma situação com o telescópio modulador de contraste, a mudança do comprimento axial foi significativamente revertida, encurtando em -9,2 mícrons (p<0,001 e p=0,002, respectivamente teste t de Student).
Conclusões: A diminuição do comprimento axial com os óculos testados neste estudo pode ser devido ao espessamento da coróide. Como o desenvolvimento da miopia para quando a coroide engrossa, esses óculos podem ser testados para controle da miopia em um ensaio clínico.
Palavras-chave: miopia, tecnologia, óculos DOT e DOMS.
Introduction
There is a growing interest in interventions to slow myopia progression in children and teenagers, with the intent of reducing the risk of high myopia-associated complications in adult life. The effect of treatment has been expressed in different ways such as axial length change in some studies or spherical equivalent change in diopters in other while some report both outcomes. This makes it difficult to compare therapies and prognosis for an individual patient, especially when studies are limited to two or three years, and do not show real life long term outcomes.
Axial elongation seems to be the preferred critical variable to assess the progression of myopia1. Although there is physiological axial elongation in emmetropic eyes during school years, and although some myopia can be classified as non-axial, studies of long-term therapies show that the elongation under myopia control treatment, will generally be less than the expected elongation without control on a given patient2.
Results in animal and human studies provide strong evidence for the short term changes in choroidal thickness produced by myopic or hyperopic defocus3-4. These can be accurately measured with modern biometry. Also, contributions of the peripheral retina to the regulation of ocular growth and refractive development have been clearly shown in animal experiments. In addition, several studies have reported relative peripheral hyperopia in myopic eyes when fully corrected with single vision lenses5-7. Currently, through different trials in myopic children, the hypothesis that the myopic defocus experienced by the retinal periphery may actually contribute to arresting progression, has been mainly proved. This was shown by the control in the progression of myopia achieved by optical devices that alter the perception of the peripheral retina through a myopic defocus and besides by a significant reduction in peripheral contrast8-16. In this way, current studies have shown that peripheral myopic defocus spectacles, diffusion optics spectacles and/or myopic defocus contact lenses have 50-60% effectiveness in arresting myopia progression in schoolchildren17-19.
There is more interest in myopia control spectacles since children aged 6-12 years old, seldom use contact lenses and they are the ones prone do develop high myopia because of their early onset. The present study tested axial length changes with Lenstar 900, tolerance and visual fields under the use of a novel and simple design with diffusion optics technology, the Diffusion Optics Multiple Segments (DOMS) Spectacle (International Optics & Ophthalmology).
The DOMS Technology is a technique based on the modulation and reduction of the peripheral contrast in a quantified and controlled manner with no impact on axial vision16. Control of myopia using another similar design of diffusion optics glasses (DOT Technology), has shown adequate efficacy and safety after 12 months in a randomized controlled study (CYPRESS Study)19. The present study was developed to test short term axial length changes using such a spectacle designed in our country.
Methods
The present study was a pilot study in consecutive myopic subjects in which we tested short time axial length changes under the use of such an especially designed spectacle with peripheral contrast modulation (Fig. 1). We also tested eye and head movements, tolerance, and visual fields under the use of this novel spectacle design. The study took place during November and December 2022. The tested glasses have a central full correction distance zone (9 mm) and a dotted peripheral contrast reduction area surrounding that central zone (Fig. 2). Subjects for this study were both genders, between 12-25 years of age, with myopic spherical equivalent between -1.00 and -5.00 diopters in either eye and with astigmatism less than -1.50 diopters in either eye, current users of glasses or contact lenses. Patients gave verbal informed consent to try a pair of especial myopia control glasses that were provided free of charge for the study that lasted approximately two hours. The Argentinian Council of Ophthalmology gave approval for this research. The ophthalmological exam included subjective refraction, intraocular pressure measurement, biomicroscopy of the anterior segment and fundus observation under dilated pupils. All myopic subjects had normal ocular exams except for their myopia.

Figure 1. Photograph showing the appearance of the DOMS technology mounted in a pair of frames.
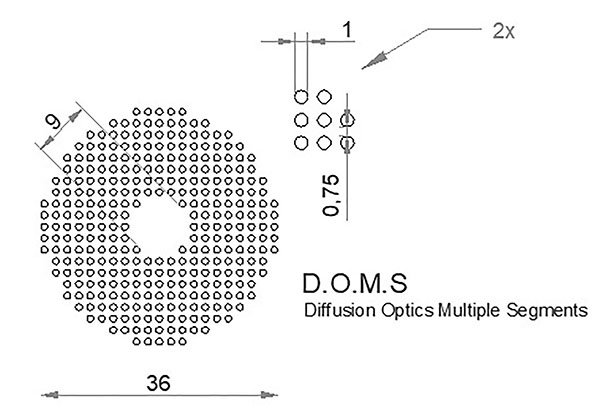
Figure 2. AutoCad design of the DOMS technology showing the dimensión and distribution of the diffusion dots.
The volunteer chose a frame for the special spectacles and the optical centering of the pupils was digitally measured in those frames (IPD Novar Device). This procedure of optical centering of the glasses in the frames was performed with special care to avoid decentering. Fifteen days later, once the especial glasses were ready, the subjects came to the office at 9 o’clock in the morning, with an indication that he/she should come rested after a good sleep, and having a light breakfast that could consist of tea or coffee with something light to eat. The subjects should be wearing the habitual corrective spectacles according to their prescription. During the whole procedure, the subjects should not drink or eat anything else, except for a sip of water, and should sit or walk briefly in a room where the experiment was performed. The experiment consisted in reading a book (PDF) with black letters on white background on a desktop computer. First reading period lasted for 20 minutes, until subjects got used to the illumination of the room with their usual glasses. Then, without any interval, 10 measurements of the axial length of the right eye were made with the Lenstar 900, Haag-Streit, Suiza (and averaged up to three decimals, deleting the deviated ones as the machine points them). Next, the subject continued reading the book on the computer for 40 minutes with their usual glasses. After this, during a short pause, a new measurement of the axial length of the right eye was made with the Lenstar 900 (10 measurements again, same procedure). Then subjects continued reading the book but this time wearing the special DOMS spectacles provided for the research study, again for another 40 minutes period. After the use of the special glasses, the third axial length measurement with Lenstar 900 was performed without a pause. After approximately two hours of work, the study ended and the volunteer could have the PDF book to finish reading the story if he/she wished so.
The statistical analysis was performed with SPSS 25 software. The means for baseline, first and second period in each subject’s right eyes were recorded and the differences up to 1 micron between pre- and post-spectacle use were calculated. Paired T-Student test were performed to find differences between pre- and post- defocus spectacle use. A p value < 0.05 was considered significant for these differences.
Results
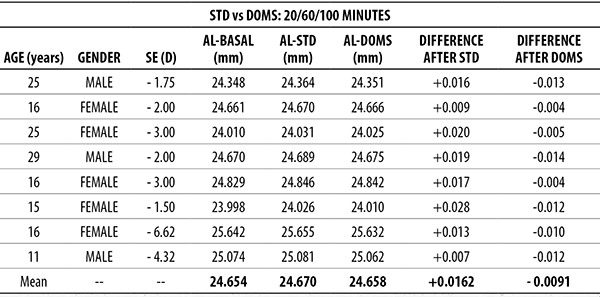
For the present study, eight (8) subjects of both genders were studied with the same protocol by two different ophthalmologists. Their mean age was 19.1 ± 6.3 years and 4 were women. Their mean spherical equivalent of their right eyes was -3.02 ± 1.72 D. The mean axial length for baseline (after 20 mins adaptation), after usual spectacles (40 mins more) and after especial contrast modulation spectacles (40 mins more) are given in Table 1. As the distributions of axial length were normal and had similar variances, paired T-Student tests were performed comparing axial length means for baseline, usual spectacles and contrast modulation spectacles. There was a significant 16.1 microns increase in axial length from baseline when reading with the usual prescription, and when this was changed to the DOMS spectacle the axial length significantly shortened by 9.2 microns (p<0.001 and p=0.002, respectively, Table 2 and Fig. 3).
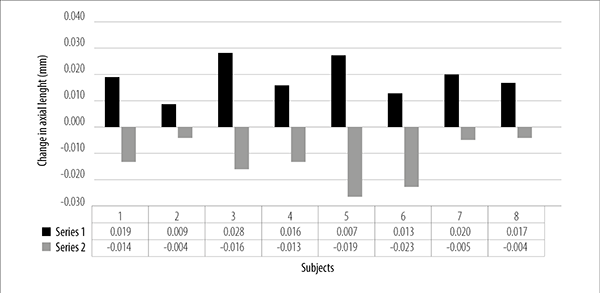
Figure 3. Axial length changes.
Table 1. Lenstar axial lengths at baseline, usual lenses and DOMS lenses.
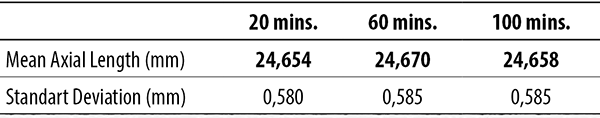
Table 2. Axial length changes with standart spectacles (STD) vs. DOMS.
After 1 month, tolerance was tested in a new interview. The subjects reported only small initial problems when the glasses were used outdoors, but these disappeared due to apparent subsequent adaptation. They were able to easily use them to work or read on the computer at the usual working distance from the desk, but had to increase their head movements to correctly follow the lines, look to the sides or their cell phone when it was in their hands. They did not report this as a big problem and were happy with the idea of using some device for myopia control. Visual fields were tested on a subject wearing regular glasses and DOMS glasses. This device shows only small changes in the peripheral visual field up to 60° without altering the central 20° away from the macula.
Discussion
This paper presents evidence of axial length changes after reading for 40 minutes with especial DOMS technology spectacles. These changes have been also shown with similar methods in human subjects under hyperopic and myopic defocus or under diluted atropine drops, while reading letters in positive or negative contrast and finally with other especial spectacles or contact lenses for myopia control. It is generally believed that these changes in axial length are indirect evidence of corresponding changes in choroidal thickness probably produced by these glasses. These changes are in line with a possible effect on myopia control, as choroidal changes precede modulation of axial elongation in myopia.
We cannot ignore the fact that choroidal thickening due to these glasses does not in itself represent evidence of their effectiveness in controlling myopia and it is also not possible to know their long-term tolerance. Therefore, we believe that a clinical trial of tolerance and efficacy would be relevant. In such a trial it would be unacceptable to have a control group left to the natural evolution of their myopia without any treatment. So, these special glasses should be tested in a non-inferiority trial against diluted atropine or already tested glass designs. Regarding the “effectiveness” and “tolerance” of these optical devices for the control of myopia, the goal should be to find an adequate balance between these two variables.
Other defocus designs evaluated by our group have shown similar axial shortening in the short term20. As this new design shows similar efficacy as the previous designs in terms of choroidal thickening and has shown very good overall tolerance even in open spaces, we are planning a long-term trial. We have also observed that in the design of these glasses with peripheral defocus or contrast modulation technology, it is necessary to optimize the centering technique of the frames, taking on account that new studies show an increase in effectiveness with smaller central areas. This makes correct centering a critical step. The effectiveness of different designs and clinical regimens for applying spectacles with contrast and defocus peripheral treatments is under study. Research in this area is promising for finding an easy and affordable treatment for myopia control.
Conclusion
The pilot testing of axial length changes during the use of novel spectacle designs produced by our local industry shows promising results in the sense that the changes in axial length reported here are in line with an effect in controlling myopia progression. A clinical trial is planned after the good results found in this study.
References