
CASE REPORTS
SLET technique in neurotrophic ulcer caused by hydroquinone with glycolic acid due to pharmaceutical dispensing error: a case report
Julieta Gancedo, Gabriela Pagano, María I. Oliva-Gómez Centurión, Leandro Emanuel Diaz-Herrera
Clínica de Ojos Dra. Mulet, Mendoza, Argentina
Received: November 2nd, 2022.
Aproved: February 12nd, 2023.
Autor corresponsal
Dr. Leandro Emanuel Díaz Herrera
Clínica de Ojos Dra. Mulet, Mendoza, Argentina
9 de Julio 2142
(5500) Ciudad de Mendoza
+54 261 420-4503
leaadiaz@gmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2023; 16(1): e76-e84.
Acknowledgements
We thank Dr. Paula Gochicoa, specialist in pediatric ophthalmology and strabismus, head of the Pediatric Ophthalmology Service of Clínica Oftalmológica Dr. Mulet, for her collaboration in the diagnosis of the patient, and Noelia Rubert, resident doctor of Ophthalmology of Clínica Oftalmológica Dr. Mulet, for her contributions to this text.
Abstract
Purpose: The technique called “Simple Limbal Epithelial Transplantation” (SLET) is useful to treat a severely damaged ocular surface. Our purpose is to present the study of a case where this occurred secondary to inadequate dispensing of a drug by the pharmacy.
Case report: We present the case of an 82-year-old woman who had Herpes zoster ophthalmicus and she suffered from severe ocular surface chemical injury secondary to a medication dispensing error by the pharmacist that gave her hydroquinone with glycolic acid (Neoquin) instead of the appropriate treatment prescribed by her doctor: ganciclovir (Neagel). After two amniotic membrane grafts and subsequent tarsal strip plus retractors reinsertion, the surgical procedure known as SLET was performed for reconstruction of the severely affected ocular surface. Complete epithelialization was observed before two weeks and at one year the ocular surface remains stable.
Conclusion: The SLET technique was effective in treating the ocular surface affected by chemical damage caused by an error in dispensing a remedy by the pharmacy.
Key words: SLET, ocular chemical injury, limbar insufficiency, ocular surface reconstruction, pharmacy dispensing errors.
Técnica SLET en la úlcera neurotrófica causada por hidroquinona con ácido glicólico debido a un error de dispensación farmacéutica: caso clínico
Resumen
Objetivo: La técnica denominada “trasplante simple de epitelio limbal” (SLET, por sus siglas en inglés) es de utilidad para tratar la superficie ocular severamente dañada. Nuestro propósito es presentar el estudio de un caso donde esto ocurrió de forma secundaria a la inadecuada dispensación de un fármaco por parte de la farmacia.
Informe de caso: Una mujer de 82 años consultó por mostrar Herpes zoster oftálmico y sufrió una grave lesión química de la superficie ocular secundaria a un error en la expedición del medicamento por parte del farmacéutico al darle hidroquinona con ácido glicólico (Neoquin) en lugar del tratamiento adecuado prescrito por su médico: ganciclovir (Neagel). Tras dos injertos de membrana amniótica y la posterior reinserción de la tira tarsal más los retractores, se realizó el procedimiento quirúrgico conocido como SLET para la reconstrucción de la superficie ocular gravemente afectada. Antes de las dos semanas se observó la completa epitelización y al año su superficie ocular se mantuvo estable.
Conclusión: La técnica de SLET fue eficaz para tratar la superficie ocular afectada por un daño químico ocasionado por un error en la dispensación de un medicamento por parte de la farmacia.
Palabras clave: SLET, lesión química ocular, insuficiencia limbar, reconstrucción de la superficie ocular, errores de dispensación farmacéutica.
Técnica SLET em úlcera neurotrófica por hidroquinona com ácido glicólico por erro de dispensação farmacêutica: caso clínico
Resumo
Objetivo: A técnica denominada "transplante de epitélio limbal simples" (SLET, por suas siglas em inglês) é útil para tratar a superfície ocular gravemente danificada. Nosso objetivo é apresentar um estudo de caso em que isso ocorreu secundário à dispensação inadequada de um medicamento pela farmácia.
Relato de caso: Uma mulher de 82 anos consultou por apresentar herpes zoster oftálmico e sofreu uma lesão química grave da superfície ocular secundária a um erro na prescrição do medicamento pelo farmacêutico ao administrar-lhe hidroquinona com ácido glicólico (Neoquin) em vez do tratamento apropriado prescrito pelo seu médico: ganciclovir (Neagel). Após dois enxertos de membrana amniótica e posterior reinserção da tira tarsal mais retratores, o procedimento cirúrgico conhecido como SLET foi realizado para reconstruir a superfície ocular gravemente afetada. A epitelização completa foi observada antes de duas semanas e após um ano sua superfície ocular permaneceu estável.
Conclusão: A técnica SLET foi eficaz para tratar a superfície ocular acometida por dano químico causado por erro na dispensação de medicamento pela farmácia.
Palavras-chave: SLET, lesão química ocular, insuficiência límbica, reconstrução da superfície ocular, erros de dispensação de medicamentos.
Background
Ocular chemical injuries in the emergency room should be considered remarkably serious pathologies that affect the ocular surface and can seriously impair the visual function. Early identification of this entity is very important for several reasons: prognosis improves with early diagnosis, improve tolerance of the treatment, better outcomes, enhance life quality1.
Therapy should promote epithelial healing, reduce inflammation, and prevent tissue melting as well as scar formation.
In those cases in which a severely compromised ocular surface associated with limbal insufficiency is presented, it may be necessary to perform a limbal transplant that will provide the essential amount of stem cells for a correct regeneration of the corneal epithelium2. The aim of the present study is to present a clinical case of a chemical lesion of the ocular surface secondary to inadequate dispensing of a drug by the pharmacy and which required surgical repair using the SLET (simple limbal epithelial transplantation) technique.
Case presentation
We present the case of an 82-year-old woman, with a personal history of glaucoma with bilateral trabeculectomy and pseudophakia in both eyes, who consulted after suffering from episodes of burning and epiphora of two days of evolution in her right eye.
Her uncorrected distance visual acuity (UDVA) was 20/20 in both eyes. The right eye examination revealed vesicular lesions in the frontal region that descended to the upper eyelid, Hutchinson’s sign, conjunctivitis, superficial keratitis, a dendritic ulcer less than 1 x 1 mm located in the inferior temporal quadrant without signs of infection (Fig. 1). The intraocular pressure was 10 mmHg in both eyes. Fundus examination showed no signs of vitreitis and a papillary diameter of 0.9 in both eyes.

Figure 1. Vesicular lesions in the frontal region that descended to the upper eyelid, Hutchinson’s sign.
Ophthalmic herpes zoster was diagnosed. Medical treatment was: 800 mg of oral acyclovir five times a day, ganciclovir ointment five times a day, vitamin complex B1, B6 and B12 once a day, tobramycin drops every six hours. The clinical course throughout admission was torpid, ten days after starting treatment the slit lamp biomicroscopy showed: senile entropion in lower eyelid of right eye (caused by the forced closure of the eye due to the pain that the patient experienced), mixed hyperemia, chemosis, conjunctival de-epithelialization with pancorneal de-epithelialization with raised edges and stromal edema. The determination of the intraocular pressure and the ocular fundus study were not possible due to the patient’s condition (Figs. 2 and 3).

Figure 2. The clinical course throughout admission was torpid, ten days after starting treatment.
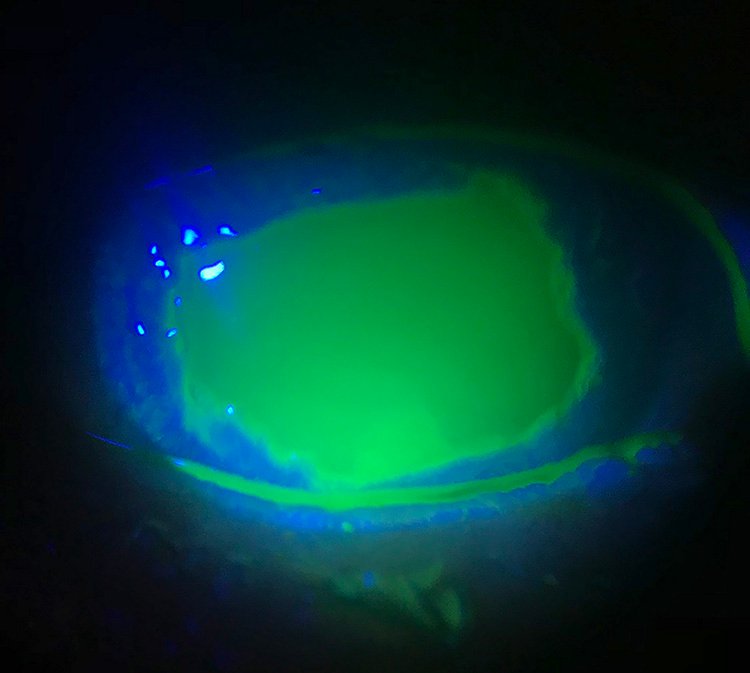
Figure 3. Mixed hyperemia, conjunctival de-epithelialization with pancorneal de-epithelialization with raised edges and stromal edema.
This evolution made us rethink several different diagnoses. The patient had been repeatedly asked to bring the medication she was using (to the doctor’s appointment), but she always forgot it. Finally, we became aware that the patient was taking hydroquinone with glycolic acid (Neoquin) whose therapeutic action is dermatological depigmentation, instead of ganciclovir (Neagel) that was the indicated treatment.
Given the diagnosis of severe ocular causticization by hydroquinone and glycolic acid, profuse irrigation with physiological saline was performed, with cleaning of necrotic tissue. The correct treatment was administered: 800 mg of oral acyclovir five times a day, ganciclovir ointment five times a day, vitamin complex B1, B6 and B12 once a day, tobramycin drops every six hours and exhaustive lubrication with dexpanthenol gel. The evolution of the corneal ulcer was torpid, and it was refractory to treatment. For this reason, it was decided to perform corneal covering with a double layer of amniotic membrane and a therapeutic corneal lens was placed to protect the membrane.
Throughout the next twelve days, central corneal de-epithelialization persisted in the right eye, with rejection of the amniotic membrane lining and therapeutic contact lens (Fig. 4). Accordingly, a new operation was performed with placement of a tarsal strip plus reinsertion of retractors to revere the entropion of the lower eyelid that complicated all types of treatment.

Figure 4. Rejection of the amniotic membrane lining, 12 day post amniotic membrane (total amniotic membrane detachment).
After this intervention, the amniotic membrane was repositioned using the SLET technique and the hemostatic adhesive (factor I, factor XIII, aprotinin, thrombin, calcium chloride) was placed, together with the therapeutic contact lenses. The patient underwent SLET technique in the right eye to restore the ocular surface, with limbal stem cells from the healthy, left eye, It is important to clarify that ten pieces of limbal tissue were grafted into the right eye. Epithelialization occurred between day 10 and 14 post SLET. The procedure had an excellent evolution and allowed the epithelial defect to be closed (Fig. 5).

Figure 5. SLET technique post-operative patient.
Currently, after 12 months of the ocular surface reconstruction procedure, the patient has an uncorrected visual acuity of 20/50 and a corrected visual acuity of 20/30. The examination highlighted the absence of epithelial defect and infections. As consequence, a diffuse interstitial keratitis has remained with attenuation of the pre-existing neovascularization (Fig. 6).
Throughout this time, the patient has maintained a topical lubricant (artificial tears and dexpanthenol gel), steroidal anti-inflammatory treatment and prophylactic herpes treatment with acyclovir 400 mg every 12 hours for 8 months.

Figure 6. SLET technical results one year after its execution.
Discussion
Corneal blindness following ocular burns was once considered incurable as it carried an extremely poor prognosis for corneal transplantation3. It has been shown that the limbus is the deposit area for stem cells and they act as a barrier against the growth of the conjunctiva on the cornea4. The term “limbal stem cell deficiency” (LSCD) refers to the reduction of limbal stem cells that maintain the corneal epithelium5.
The destruction of limbal epithelium by chemical, thermal, and other widespread ocular surface injuries is important to clinically recognize and explains the development of abnormal ocular surface problems of recurrent and persistent corneal epithelial defects, chronic inflammation, stromal neovascularization, and presence of goblet cells (conjunctivalization) on the corneal surface. Collectively, these abnormalities indicate a defect or absence of conjunctival transdifferentiation and imply the absence of limbal epithelium6.
Clinically, the causes of LSCD can be divided into Hereditary: aniridia (bilateral) keratitis associated with multiple endocrine deficiency (bilateral); and acquired: Stevens-Johnson syndrome (bilateral), chemical injuries (unilateral/bilateral), contact lens-induced keratopathy (unilateral/bilateral), microbial keratitis, post-surgical or post-radiotherapy lesions, squamous neoplasia of the ocular surface (OSSN), eyelid abnormalities, persistent epithelial defects and, symbepharon7-8. It is known that although we could perform a corneal transplant in these patients to restore vision, the pre-existing vascularization is associated with a high rate of graft rejection9.
Simple limbal epithelial transplantation (SLET) is a surgical technique first described by Dr. Sangwan in 2012 at the L V Prasad Eye Institute, Hyderabad, India, for the treatment of limbal stem cell deficiency (LSCD)8. This technique consists of transplantation of limbal stem cells from the healthy eye contralateral to the lesion of the diseased eye using the help of the amniotic membrane that is placed on the corneal surface of the affected eye, from which the pannus generated by the cell deficiency was previously removed (Figs. 5 and 6). Since then, several papers have validated its efficacy restoring the ocular surface, renewing the corneal epithelium and avoiding the re-conjunctivalization of the cornea10. SLET has shown to be an efficient and cost-effective surgical technique for the restoration of the ocular surface even in cases with severe burns and complete LSCD11-12.
Moreover a dispensing error is a discrepancy between a prescription and the medicine that the pharmacy delivers to the patient or distributes to the ward on the basis of this prescription, including the dispensing of a medicine with inferior pharmaceutical or informational quality13. Each year, in the United States alone, 7,000 to 9,000 people die due to a medication error14. Additionally, hundreds of thousands of other patients experience but often do not report an adverse reaction or other complications related to a medication.
Finally, a major consequence of medication errors is that it leads to decreased patient satisfaction and a growing lack of trust in the healthcare system14.
Conclusion
Throughout this article, reference has been made to the various therapeutic solutions used to deal with the complications that successively developed. An error in dispensing a drug by the pharmacy can have severe ophthalmological consequences, and throughout this article, reference has been made to the different therapeutic solutions that have been necessary to solve the problems that this caused. The use of hydroquinone with glycolic acid topically in the eye caused an acid caustication that severely affected the cornea. After multiple procedures with grafts of amniotic membrane and tarsal strip plus reinsertion of retractors, it was necessary to perform the SLET surgical technique to finally obtain the adequate reconstruction of the severely affected ocular surface.
With the present report we hope to contribute to the dissemination of the SLET technique to solve severe ocular surface problems, but in addition, we want to emphasize the importance of checking drugs before using them in the eyes by patients, and emphatically that more precautions should be taken in pharmacies when dispensing drugs.
References