ARTÍCULO ORIGINAL
Stereopsis evaluation in patients under pharmacological treatment for presbyopia
Giovanna Benozzia, Sonia Facala, Juliana Leiroa, Cristian Pereza, Betina Ormanb
aCentro de Investigación Avanzada de la Presbicia, Buenos Aires, Argentina.
bCátedra de Farmacología de la Facultad de Odontología de la Universidad de Buenos Aires, Argentina.
Received: April 13rd, 2020.
Aproved: May 12nd, 2020.
Corresponding author
Betina Orman, PhD
Pharmacology Unit
Facultad de Odontología, Universidad de Buenos Aires
M. T. de Alvear 2142, 4th Floor B
(1122AAH) Buenos Aires, Argentina
+54 11 5287 6235
betina.orman@odontologia.uba.ar
Oftalmol Clin Exp (ISSN 1851-2658)
2020, 13(2): 82-89.
ABSTRACT
Objective: Stereopsis is the binocular perception of depth, which has been associated to the improvement in near visual acuity. Presbyopia is the progressive weakening of accommodation, which could be modulated by an eye-drop pharmacological treatment (Benozzi’s method). The purpose of this work was to evaluate stereopsis in patients treated with Benozzi's method for presbyopia.
Methods: A non-randomized case-series prospective study was developed. Twenty emmetropic patients were included, in the range from 40 to 55 years old. Different parameters were measured, such as spherical equivalent refraction (SE), uncorrected and corrected distance and near visual acuity (UDVA-CDVA/UNVA-CNVA), ocular motility and stereopsis. Measurements were performed in three situations: at baseline, with optical correction (eyeglasses) and, after 30 minutes of treatment (eye-drops instillation).
Results: The mean SE refraction in the right eye was 0.34 ± 0.32D and in the left eye it was 0.23 ± 0.22D. Orthophoria was found in 85% of patients while 15% had exophoria. The mean UNVA was 0.197 ± 0.02 LogMAR; with optical correction achieved J1 (0 LogMAR) and after treatment, the mean UNVA was 0.02 ± 0.06 LogMAR (18 cases with J1 and 2 with J2). Pre-treatment mean stereopsis was 200.5 ± 190.85 s of arc, which improved to 52.5 ± 19.70 s of arc (p<0.0018) after the optic correction and to 58±22.38 s of arc (p<0.002) after pharmacological treatment. Both methods exhibited similar results by Titmus stereoscopic tests showing no statistically significant difference (p>0.41).
Conclusions: This study demonstrates that pharmacological treatment for presbyopia not only re-established near and distance visual acuity but restored stereopsis.
Keywords: Stereopsis, presbyopia, pharmacological treatment, stereoacuity.
Evaluación de la estereopsis de pacientes en tratamiento farmacológico de la presbicia
RESUMEN
Objetivo: La estereopsis es la percepción binocular de profundidad que está asociada a la mejoría de la visión cercana. El objetivo del presente trabajo fue evaluar la estereopsis en los pacientes tratados con el Método Benozzi, que es un tratamiento farmacológico para la presbicia.
Métodos: Se desarrolló un estudio prospectivo, no randomizado, de una serie de casos en 20 pacientes emétropes de 40 a 55 años. Se evaluaron: equivalente esférico (ES), agudeza visual (AV) de lejos y cerca, con y sin corrección, motilidad ocular y estereopsis. Se realizaron las mediciones sin y con corrección óptica de cerca y 30 minutos luego de realizar el tratamiento.
Resultados: El valor medio del ES fue de 0.34 ± 0.32D en ojos derechos y de 0.23 ± 0.22D en ojos izquierdos. El 15% presentaba exoforia y se encontró ortoforia en el resto. El valor medio de la AV cercana s/c fue de 0.197 ± 0.02 LogMAR y de 0.02 ± 0.06 LogMAR (18 casos con J1 y dos con J2) con tratamiento. Con el uso de anteojos todos obtuvieron J1 (0 LogMAR). El valor medio de la estereopsis antes del tratamiento fue de 200,5 ± 190,85 s de arco, que mejoró luego de la corrección óptica a 52,5 ± 19,70 s de arco (p<0.0018), y luego del tratamiento con Método Benozzi a 58 ± 22,38 s de arco (p<0.002). La estereopsis no mostró diferencias estadísticamente significativas entre los anteojos y el tratamiento (p>0.41).
Conclusiones: Este estudio demuestra que el tratamiento farmacológico para la presbicia no sólo mejora la visión de cerca, mientras mantiene la visión de lejos, sino que también mejora la estereopsis.
Palabras clave: estereopsis, presbicia, tratamiento farmacológico.
Avaliação da estereopsia de pacientes em tratamento farmacológico da presbiopia
RESUMO
Objetivo: A estereopsia é a percepção binocular de profundidade que está associada com a melhoria da visão de perto. O objetivo do presente trabalho foi avaliar a estereopsia nos pacientes tratados com o Método Benozzi, que é um tratamento farmacológico para a presbiopia.
Métodos: Desenvolveu-se um estudo prospectivo, não randomizado, de uma série de casos em 20 pacientes emétropes de 40 a 55 anos. Avaliaram-se: equivalente esférico (ES), acuidade visual (AV) de longe e perto, com e sem correção, motilidade ocular e estereopsia. Realizaram-se as medições sem e com correção óptica de perto e 30 minutos logo de realizar o tratamento.
Resultados: O valor médio do ES foi de 0.34 ± 0.32D em olhos direitos e de 0.23 ± 0.22D em olhos esquerdos. 15% apresentava exoforia e se encontrou ortoforia no resto. O valor médio da AV próxima s/c foi de 0.197 ± 0.02 LogMAR e de 0.02 ± 0.06 LogMAR (18 casos com J1 e dois com J2) com tratamento. Com o uso de óculos todos obtiveram J1 (0 LogMAR). O valor médio da estereopsia antes do tratamento foi de 200,5 ± 190,85 s de arco, que melhorou logo da correção óptica a 52,5 ± 19,70 s de arco (p<0.0018), e logo do tratamento com Método Benozzi a 58 ± 22,38 s de arco (p<0.002). A estereopsia não mostrou diferencias estatisticamente significativas entre os óculos e o tratamento (p>0.41).
Conclusões: Este estudo demostra que o tratamento farmacológico para a presbiopia não melhora apenas a visão de perto, enquanto mantem a visão de longe, mas também melhora a estereopsia.
Palavras chave: estereopsia, presbiopia, tratamento farmacológico.
INTRODUCTION
With aging decrease visual performance, as happens with the “presbyopia”, which is the progressive weakening of accommodation resulting in loss of the visual ability to focus on objects situated at different distances1 . As presbyopia, other ocular functions deteriorate with aging like stereopsis. Stereopsis is the binocular perception of depth and it has been disclosed to improve with better near visual acuity2. Moreover, with concerns to its functional significance, it has been reported to be a significant risk factor for self-reported visual disability with aging3. Good stereoacuity impact the performance on certain motor necessary for ordinary tasks that implicate precise manipulation of objects within near range as threading a needle4. In concern to the affection of stereopsis in the large disparity range, is important to support depth judgments at distances up to 200m as5, manage through the environment, up and down stairs and obstacle prevention6.
Actually, presbyopia treatments have inherence on stereopsis. Within the plethora of treatments for presbyopia there are different strategies that could involve spectacles, contact lenses, surgical correction, and the innovative pharmacological treatment7-8. Corneal refractive surgery includes monovision or multifocality created by excimer ablation, conductive keratoplasty, and diverse inlays. Other surgical correction can be intraocular lens replacement using either monofocal implants for monovision, multifocal lenses, accommodative implants, and extended depth of focus lenses (EDOF)9.
The pharmacological treatment (Benozzi’s Method®: patents US 8.524.758 B2 and EP1.938.839 B1 among others) consists of topical daily eyedrops in both eyes with a combination of pilocarpine and diclofenac1. Pilocarpine, as a parasympathetic agonist, produces a spasmodic contraction of the ciliary muscle and miosis10. Diclofenac is a non-steroid anti-inflammatory drug (NSAID). This combination of NSAIDs and parasympathetic agonists permits the decrease in the intensity of the contraction of the ciliary muscle and the pupil, changing the shape and position of the lens obtaining focus at all distances restoring accommodation11.
Spectacles are the classic method to treat presbyopia as in known that maintain binocularity and stereopsis. Taking into account that the pharmacological treatment restores accommodation and preserves binocularity, the aim of this study is to evaluate stereopsis in patients treated with the pharmacological treatment for presbyopia.
MATERIALS AND METHODS
Study design
A non-randomized case-series prospective study was developed, including 20 patients with presbyopia treated with pharmacological treatment for presbyopia “Método Benozzi”, from March to June 2019. The study was performed following the tenets of Helsinki, in a private ophthalmology clinic (Centro de Investigación Avanzada de la Presbicia) in Buenos Aires city, Argentina. An informed consent was obtained from every patient. The present study protocol was evaluated and approved by the Ethical Committee of the Argentinian Presbyopia Society (0001/2019).
Exclusion and inclusion criteria, parameters to evaluate and statistics.
All patients were studied following a complete ophthalmic baseline assessment. The examination scheme included uncorrected distance visual acuity (UDVA), uncorrected near visual acuity (UNVA), corrected distance visual acuity (CDVA), and corrected near visual acuity (CNVA), ocular motility and stereopsis. Stereopsis was assessed at baseline, with optical correction with eyeglasses and for last, with the pharmacological treatment for presbyopia 30 minutes after the instillation of the eye-drops.
1. Patients age between 40 to 55 years old; 2. Refractive errors were measured (auto-refracto-keratometer; Nidek ARK700K) and patients were excluded if one of the eyes has a cycloplegic spherical refraction greater than -0.50 D or 1.0 D and/or with cylinder refraction higher than 1.0 D; 3. The uncorrected distance visual acuity (UDVA) was measured with Snellen charts and converted to the logarithm of the minimum angle of resolution (logMAR) and uncorrected near visual acuity (UNVA) was measured with reading chart at 45 cm distance (objectively measured), with Jaeger (J) standard notation (from J1 to J8). If binocular UDVA was lower than 20/40, patients were excluded; 4. Patients with amblyopia, history of any kind of glaucoma, pseudophakia, macular disease or any retinal disorder, or had a history of ophthalmological diseases were also excluded.
Stereopsis test
The stereoacuity under natural light was evaluated using the Titmus Stereopsis Test (Stereo Optical Co., Chicago, IL, USA). When testing, subjects viewed the images through polarizing spectacles with 40 cm distance and held perpendicular to the visual axis. The booklet comprises of a large-disparity fly, three series of animals, and nine sets of circles. The fly and the series of circles are used in adults meanwhile the series of animal are usually used for children. The fly was shown first to determine the presence of gross stereopsis. If a positive response was given, the series of circles test continued to stipulate a finely graded sequence for critical testing. Each circle set are comprised by 4 circles, and only one of them seems to be closer to subjects than others (3D). A total of 9 levels, ranging from 40 to 800 seconds of arc, are applied in circle test. With the decrease of the degree of crossed disparity, the difficulty level in stereopsis increases. Stereoacuity is recorded with the most difficult level achieved by patients.
Statistical analysis
Quantitative data are presented as mean ± standard deviation. Differences of means were analyzed using paired sample t test. A value of p <0.05 was considered statistically significant in all tests. Statistics were calculated using was performed using GraphPad Prism version 7.00 for Windows, GraphPad Software, La Jolla California, USA.
RESULTS
20 presbyopic patients were studied, of whom 9 were women and 11 men. The mean age was 49.7 ± 4.1 years. They were all emmetropic patients with spherical equivalent refraction in the right eye 0.34 ± 0.32D and in the left eye 0.23 ± 0.22D. In relation to ocular motility, 85% of patients (17 cases) had orthophoria while 15% (3 cases) had exophoria.
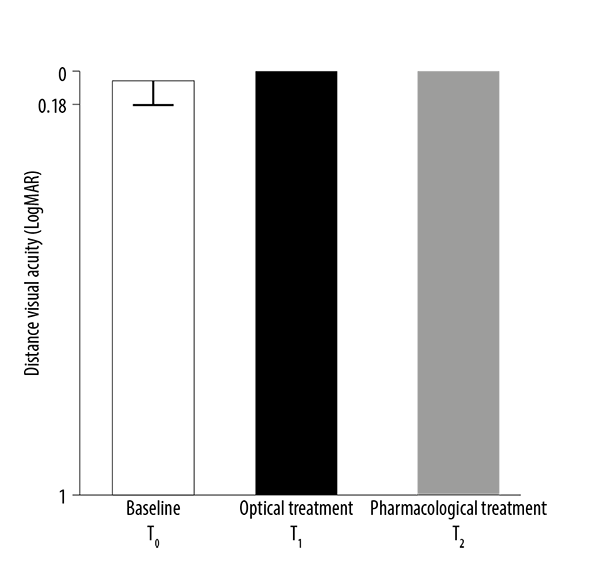
Figure 1 shows distance visual acuity with and without treatment. Considering that the patients included in the study were emmetropic they presented a very good UDVA of 0.019 ± 0.01 LogMAR. All the patients reached CDVA of 0 LogMAR (20/20 Snellen) both when treated with optical correction with eyeglasses and with pharmacological treatment.
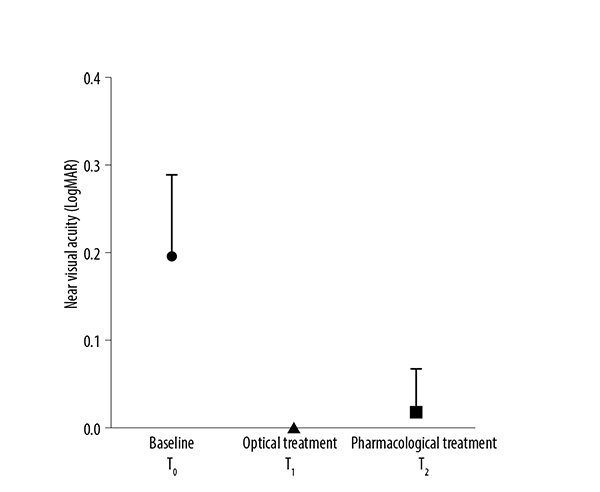
In figure 2, near visual acuity with and without treatment is observed. The mean UNVA was 0.197 ± 0.02 LogMAR without treatment. All the patients with optical treatment achieved a CNVA of J1 (0.0 LogMAR) whereas when treated with the pharmacological treatment, all the patients achieved 0.02 ± 0.06 LogMAR (18 cases with J1 and 2 with J2).
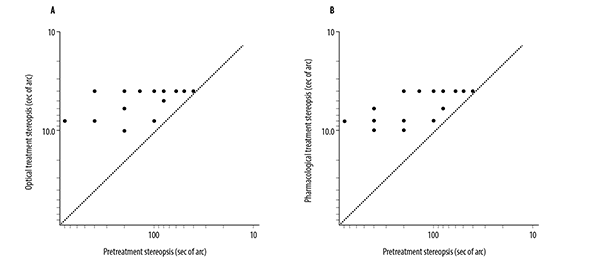
Stereopsis testing, as measured by Titmus stereoscopic tests, is shown in figure 3. Pre-treatment mean stereopsis was 200.5 ± 190.85s of arc which improved to 58 ± 22.38 s of arc (p<0.002) after pharmacological treatment (Figure 3A) and to 52.5 ± 19.70 s of arc (p<0.0018) after the optical correction procedure (Figure 3B). Both methods exhibited similar results by Titmus stereoscopic tests showing no statistically significant difference (p>0.41).
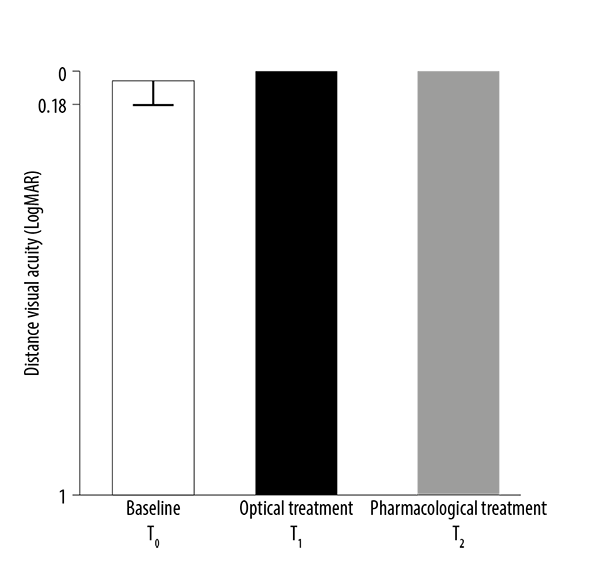
Figure 1. Distance visual acuity with and without treatment. Baseline (T0) uncorrected distance visual acuity, with eyeglasses (T1) and with pharmacological treatment (T2).
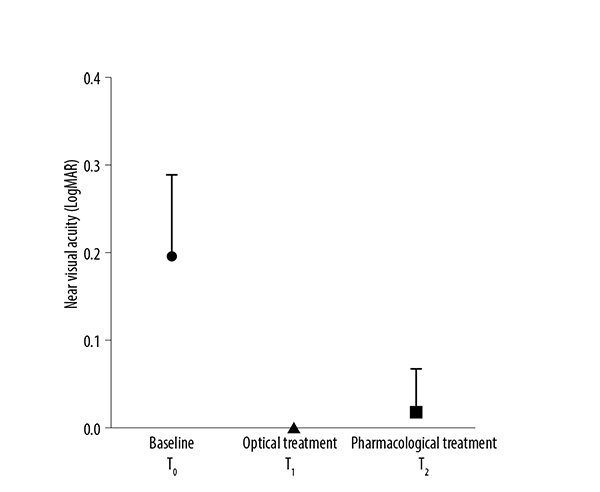
Figure 2.Near visual acuity with and without treatment. Baseline (T0) uncorrected distance visual acuity, with eyeglasses (T1) and with pharmacological treatment (T2).
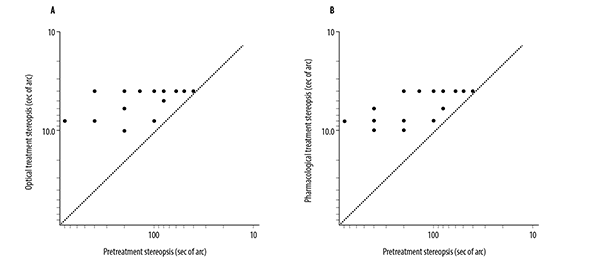
Figure 3. Stereopsis evaluation by Titmus Stereoscopic Test. A: Stereopsis was evaluated at baseline (T0) and optical correction with eyeglasses (T1). B: Stereopsis was evaluated at baseline (T0) and after pharmacological treatment (T2).
DISCUSSION
Stereopsis is developed from the early infancy and is gradually lost as accommodation decreases. The reduced level of stereopsis has a substantial impact on visuomotor tasks and difficulties in locomoting safely, among others. The present study demonstrates in 20 emmetropic presbyopic patients that pharmacological treatment for presbyopia restored near and distance visual acuity reached 20/20 and J1, respectively, as well as optical treatment. Examination of the results of stereopsis by Titmus stereoscopic tests indicated that all patients improved stereoacuity by both methods showing no statistical differences between them.
At birth, the visual system (included the components of the eye and the neural circuit patterns) is immature and during the first postnatal months begins its dynamic development. There are three critical stages in visual system maturity: development, sensitive and recovery, taking into account that the timing of each period depends on each specific visual function12. In concern to stereopsis is not present at birth and progresses according visual acuity improves. Fox et al. in 1980 reported that stereopsis emerges from 3.5 to 6 months from an investigation in infants based on attracting baby’s attention through the apparent motion in visual space of a stereoscopic contour contained within a random-element stereogram13. Biagi et al. in 2015, provided the first maps of visual cortical function in human infants by functional magnetic resonance imaging (fMRI)14. The study lightered up that the associative regions of the cortex responsible for motion processing react similarly in 7-week-olds and adults. However, the development of functional connections between the associative areas and the primary visual cortex is not yet mature14. The stereopsis development stage starts from around three months of age, with a rapid progression during the first year and improvement over the first five years of life where neural plasticity is in the apex15. The sensitive stage could extend to maturity, regarding that neural plasticity decreased according growing up12.
During the first years of childhood, the human being presents a maximum of 15 adaptive diopters, however, for most visual tasks the need for accommodation is much lower16. Although the amplitude of accommodation decreases gradually until approximately 65 years, when it is almost completely lost, the deficit in most people seems to have a sudden onset and presbyopia appears. According Helmholtz’s theory of accommodation17, presbyopia is defined as the gradual loss of accommodation with aging consequential to loss of elasticity of the lens capsule and substance. Accommodation in humans is achieved by ciliary muscle and iris sphincter contractions, convergence and variations in the shape and position of the lens18. When ciliary muscles contract during accommodative action it release tension on the zonules allowing the elastic lens capsule to reshape and change the dioptric power of the lens. The different subtypes of muscarinic receptors on iris and ciliary muscle are stimulated by the cholinergic neurotransmitter, acetylcholine19.
The improvements in stereopsis for patients who underwent pharmacological treatment were significant, especially because other presbyopia treatments available to date have diminished stereopsis and binocularity in some degree20.
Monovision used for presbyopic correction is a well-established method with one eye corrected for near vision and the other eye for distance vision. There are many ways to accomplished monovision, using contact lenses, laser in situ keratomeleusis (LASIK) treatment of monovision (approved by FDA in 2007)20, and using intraocular monocular implants. The non-dominant eye is corrected for near vision and the dominant eye for distance vision. Nevertheless, the complex visual system is intended to consent both eyes to work together to obtain information from the background. Human visual field overlaps in nearly 60 per cent and where a sacrifice of a greater peripheral vision is made in favor of information provided by binocular disparity, and this results in welfares to functional ability12.
Monovision is in the edge of the brain to create stereopsis21. When the retinal images formed on each eye disagree, stereopsis is affected and different approaches have been widely studied in the past. Former literature relates asymmetric changes in the contrast of the two retinal images to degradation of stereopsis22. Latest revisions have searched the role of aberrations, outside defocus and astigmatism when they are unequal in the two eyes, over stereopsis23.
Monovision intentionally decreases contrast sensitivity, binocularity and stereopsis20 that is why the selection of the patient is essential. Inappropriate patients include aviators, professional drivers, writers and those who spend all day on computers20. Binocular vision is fundamental for stereopsis and, applying monovision, stereopsis can be seriously compromised24.
Regarding corneal inlay influence on stereopsis, it has not been widely studied25 but the results of the experiment realized by Fernández et al. 2013 showed that a small aperture as a corneal inlay, can produce similar values of stereoacuity to those attained only under photopic conditions24. These results are not the same under scotopic situations.
Has also been shown that multifocality achieved through contact lenses, sophisticated spectacles, corneal correction or intraocular implants reduces stereoacuity, although it is vaguely better than with monovision26. While technology is rapidly improving and there are very sophisticated lens options for presbyopes, none offer the range and quality of vision achieved by a young eye with active accommodation27.
Surgical corneal presbyopic correction attempts to create a bifocal cornea, but this procedures carry risks of scarring, night vision problems and vision loss9, in addition to loss of binocularity and stereopsis20. The same happens with lenticular procedures in addition to the risks of night vision problems, glare, halos, and endophthalmitis28. Besides accommodating implants theoretically could have reduced effects on binocularity and stereopsis, all this procedures are quite invasive, they may be more appropriate for cataract patients29.
Patients under pharmacological treatment recovered both distance and near visual acuity, as proved in this study. Maintaining binocular vision is essential for stereopsis. Moreover, we can observe improvement of stereopsis in the patients treated with the eye drop. This enhancement can be observed as long as the effect on visual acuity. Among the different treatments for presbyopia available, the relevance of the results is evaluated in relation to a range of outcomes, where optical treatment with eyeglasses and pharmacological treatment achieved to reestablish stereopsis. This point is essential when is proven that a reduced range of stereopsis has a negative influence on the ability to perform several tasks, and can lead to an increase in trouble relating in the real world. The diminution in stereoacuity affects performance in complex spatial-motor activities, resulting in difficulties in ordinary life.
CONCLUSION
Finally, in a recent publication, the presented treatment has shown efficacy and safety in an eight-year retrospective study30. In the present work, this pharmacological treatment proved to ameliorate stereopsis as well as optical treatment taking to account that both methods conserve binocularity, necessarily condition for stereopsis, in contraposition with other strategies that intents to correct presbyopia. Taken together, these observations demonstrate that pharmacological treatment for presbyopia not only reestablished near and distance visual acuity but restored stereopsis.
REFERENCES
1. Facal S, Leiro J, Gualtieri A, Perez C, Benozzi G, Orman B. Ocular surface evaluation in patients treated with pharmacological treatment for presbyopia. Int J Ophthalmic Pathol 2018; 7.
2. Donzis PB, Rappazzo JA, Bürde RM, Gordon M. Effect of binocular variations of Snellen’s visual acuity on titmus stereoacuity. Arch Ophthalmol 1983; 101: 930-932.
3. Wubben TJ, Guerrero CM, Salum M et al. Presbyopia: a pilot investigation of the barriers and benefits of near visual acuity correction among a rural Filipino population. BMC Ophthalmol 2014; 14: 9.
4. McKee, SP. The spatial requirements for fine stereoacuity. Vision Res 1983; 23: 191-198.
5. Allison RS, Gillam BJ, Palmisano SA. Binocular slant discrimination beyond interaction space [abstract]. J Vis 2008(6): 536, doi:10.1167/8.6.536.
6. Smith CE, Allison RS, Wilkinson F, Wilcox LM. Monovision: consequences for depth perception from large disparities. Exp Eye Res 2019; 183: 62-67.
7. Chou B. Presbyopia eye drops are in sight [online]. Englewood, CO: Review Education Group, 2018. Retrieved from: https://www.revieweducationgroup.com/ce/presbyopia-eye-drops-are-in
8. Grzybowski A, Mimier M, Misiuk-hojło M. Farmakologiczne metody leczenia starczowzroczności. OphthaTherapy 2017; 4: 237-240, doi: 10.24292/01.OT.291217.07.
9. Hipsley A, Ma DHK, Sun CC et al. Visual outcomes 24 months after LaserACE. Eye Vis (Lond) 2017 , 4: 15.
10. Ostrin LA, Glasser A. Comparisons between pharmacologically and Edinger-Westphal-stimulated accommodation in rhesus monkeys. Invest Ophthalmol Vis Sci 2005; 46: 609-617.
11. Benozzi J, Benozzi G, Orman B. Presbyopia: a new potential pharmacological treatment. Med Hypothesis Discov Innov Ophthalmol 2012; 1: 3–5.
12. O’Connor AR, Tidbury LP. Stereopsis: are we assessing it in enough depth? Clin Exp Optom 2018; 101: 485-494.
13. Fox R, Aslin RN, Shea SL, Dumais ST. Stereopsis in human infants. Science 1980; 207: 323-324.
14. Biagi L, Crespi SA, Tosetti M, Morrone MC. BOLD response selective to flow-motion in very young infants. PLoS Biol 2015; 13(9)=:e1002260.
15. Ciner EB, Schanel-Klitsch E, Herzberg C. Stereoacuity development: 6 months to 5 years: A new tool for testing and screening. Optom Vis Sci 1996; 73: 43-48.
16. Katz M, Kruger PB. The human eye as an optical system. In: Duane TD, Tasman W, Jaeger EA (eds.). Duane’s Ophthalmology. Philadelphia: Lippincott Williams & Wilkins, 2009, v.1, cap. 33.
17. Helmholtz von, HH. Mechanism of accommodation. In: Southall JPC (ed.). Helmholtz’s Treatise on physiological optics. Baltimore: The Optical Society of America, 1924, p. 143–172.
18. Benozzi G, Leiro J, Facal S et al. Developmental changes in accommodation evidenced by an ultrabiomicroscopy procedure in patients of different ages. Med Hypothesis Discov Innov Ophthalmol 2013; 2: 8-13.
19. Koeppl C, Findl O, Kriechbaum K, Drexler W. Comparison of pilocarpine-induced and stimulus-driven accommodation in phakic eyes. Exp Eye Res 2005; 80: 795-800.
20. O’Keefe M, O’Keeffe N. Corneal surgical approach in the treatment of presbyopia. J Clin Exp Ophthalmol 2016; 7: 1-4.
21. Menassa N, Fitting A, Auffarth GU, Holzer MP. Visual outcomes and corneal changes after intrastromal femtosecond laser correction of presbyopia. J Cataract Refract Surg 2012; 38: 765-773.
22. Jain S, Arora I, Azar DT. Success of monovision in presbyopes: review of the literature and potential applications to refractive surgery. Surv Ophthalmol 1996; 40: 491-499.
23. Schor C, Landsmant L, Erickson P. Ocular dominance and the interocular suppression of blur in monovision. Am J Optom Physiol Opt 1987; 64: 723-730.
24. Fernández EJ, Schwarz C, Prieto PM et al. Impact on stereo-acuity of two presbyopia correction approaches: monovision and small aperture inlay. Biomed Opt Express 2013; 4: 822-830.
25. Dexl AK, Seyeddain O, Riha W et al. Reading performance after implantation of a small-aperture corneal inlay for the surgical correction of presbyopia: two-year follow-up. J Cataract Refract Surg 2011; 37: 525-531.
26. Richdale K, Mitchell GL, Zadnik K. Comparison of multifocal and monovision soft contact lens corrections in patients with low-astigmatic presbyopia. Optom Vis Sci 2006; 83: 266-273.
27. Chu BS, Wood JM, Collins MJ. Effect of presbyopic vision corrections on perceptions of driving difficulty. Eye Contact Lens 2009; 35: 133-143.
28. Imbeau L, Majzoub S, Thillay A et al. Presbyopia compensation: looking for cortical predictors. Br J Ophthalmol 2017; 101: 223-226.
29. Macsai MS, Padnick-Silver L, Fontes BM. Visual outcomes after accommodating intraocular lens implantation. J Cataract Refract Surg 2006; 32: 628-633.
30. Benozzi G, Perez C, Leiro J, Facal S, Orman B. Presbyopia treatment with eye drops: an eight year retrospective study. Trans Vis Sci Tech. In press, https://doi.org/10.1167/tvst.0.0.2246