
CASE REPORT
Cataract by electrocution
Guillermo Raúl Vera Duarte, Eliana Duarte Fariña, Martín Arrúa, Luis González
Cátedra de Oftalmología, Hospital de Clínicas, Universidad Nacional de Asunción, Paraguay.
Received: November 8th, 2021.
Aproved: April 23rd, 2022.
Autor corresponsal
Dr. Guillermo Vera Duarte
guillermoveraduarte@gmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2022; 15(2): e218-e222.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent
The patient gave her informed written consent to publish the case and the images.
Abstract
Objective: Electrical burns generate a special type of injury the longer a person is exposed to electricity, the worse the injuries will be. Cataracts resulting from this mechanism are of low frequency, because of that our purpose is to present a cataracts case by electrocution.
Case report: A 22-year-old male patient, from a rural area, a gardener by profession, with a history of electrocution with loss of consciousness for approximately 2 hours, was hospitalized and placed under surveillance for 1 month. His vision worsened over time, which led him to the ophthalmology consultation, 4 months after. A cataract was detected in his right eye. Phacoemulsification was performed with trypan blue capsular staining prior to capsulorhexis and implantation of a foldable intraocular lens (IOL) in a capsular bag, without complications. On the 5th postoperative day of the right eye, a transparent corneal, slight inflammation, IOL in the capsular bag, a 20/20 visual acuity without correction was observed.
Conclusion: The formation of cataracts secondary to electrocution is possible, because of that as soon as the patient is stable should have a complete routine ophthalmology evaluation. Generally, these cases, without previous affections is considered to have a good visual prognosis, as was described in this work.
Key words: cataracts, traumatic cataract, electrocution.
Catarata por electrocución
Resumen
Objetivo: Las quemaduras eléctricas producen un daño asociado al tiempo de exposición de la persona a la electricidad. Las cataratas ocurridas por este mecanismo son de baja frecuencia, por lo cual nuestro propósito es presentar un caso de cataratas por electrocución.
Caso clínico: Un hombre de 22 años, jardinero oriundo de una zona rural, tuvo un accidente eléctrico con pérdida de consciencia durante aproximadamente 2 horas, por lo que fue hospitalizado y puesto en observación durante 1 mes. Su visión fue empeorando con el tiempo, lo que originó su consulta oftalmológica 4 meses después. Se le detectó una catarata en su ojo derecho. Se le realizó facoemulsificación utilizando azul tripán para teñir la cápsula antes de realizar la capsulorrexis y se le implantó una lente intraocular plegable en el saco capsular, sin complicaciones. Al quinto día de la cirugía tenía la córnea trasparente, ligera inflamación, la lente en su lugar y una agudeza visual sin corrección de 20/20.
Conclusión: La formación de cataratas secundarias a electrocución es posible, por lo tanto, en cuanto el paciente esté estable deberá realizar un control oftalmológico completo. Generalmente estos casos donde no hay afecciones previas tienen un buen pronóstico visual.
Palabras clave: cataratas, cataratas traumáticas, electrocución.
Catarata por eletrocussão
Resumo
Objetivo: As queimaduras elétricas produzem danos associados ao tempo de exposição da pessoa à eletricidade. As cataratas causadas por esse mecanismo são de baixa frequência, portanto o objetivo é apresentar um caso de catarata por eletrocussão.
Caso clínico: Homem de 22 anos, jardineiro da zona rural, sofreu acidente elétrico com perda de consciência por aproximadamente 2 horas, pelo qual foi internado e mantido em observação por 1 mês. A sua visão piorou ao longo do tempo, o que levou à sua consulta oftalmológica 4 meses depois. Uma catarata foi detectada em seu olho direito. A facoemulsificação foi realizada com azul de tripano para coloração da cápsula antes da capsulorrexe, e uma lente intraocular dobrável foi implantada no saco capsular sem complicações. No quinto dia de pós-operatório, apresentava córnea transparente, leve inflamação, lente no lugar e acuidade visual não corrigida de 20/20.
Conclusão: A formação de catarata secundária à eletrocussão é possível, portanto, assim que o paciente estiver estável, deve ser realizado um controle oftalmológico completo. Geralmente, esses casos em que não há condições prévias têm um bom prognóstico visual.
Palavras-chave: catarata, catarata traumática, eletrocussão.
Introduction
Electrical burns generate a special type of injury, derived from the physical properties of electricity and the path of current flow through tissues and organs, causing superficial or multi-organ involvement1-2. The path that the current takes in the body usually determines the possible tissues that will be affected2.
The hand being the most frequent point of contact of the electrical source, the second is the head3. The longer a person is exposed to electricity, the worse the injuries will be. Cataracts resulting from this mechanism are of low frequency2,4.
Cataract is a clouding of the lens that can be due to a variety of causes5. These include traumatic cataracts, which may be due to different mechanisms such as related to foreign body injury to the lens or blunt trauma to the eyeball. And rarer causes from excessive exposure to heat, X-rays, radiation therapy, radioactive materials, and electricity5.
The case of a patient with the diagnosis of cataract due to electrocution is presented, which manifested with loss of visual acuity months after an electrocution event.
Case report
A 22-year-old male patient, from a rural area, a gardener by profession, with a history of electrocution with loss of consciousness for approximately 2 hours, was hospitalized and placed under surveillance for 1 month; he required reconstructive surgeries at the level of the right hemisphere due to injuries typical of the accident, and a supratrochlear amputation of the right leg was performed (Figs. 1, 2).

Figure 1. Secondary lesions at the level of the hemicranium.

Figure 2. Supratrochlear amputation of the right leg.
He visited the ophthalmology service 4 months after the event due to a history of progressive decrease in visual acuity in the right eye. The physical examination revealed a significant leukocoria of the right eye, scarring lesions at the level of the right hemisphere and amputation of the right MI. In the ophthalmological evaluation of the right eye, a visual acuity of hand movement without improvement, intraocular pressure (IOP) 12 mmHg, positive photomotor reflex and as soon as the anterior segment was observed a clear conjunctiva, transparent cornea, anterior chamber formed, wide and white cataract with opacities at the level of the anterior capsule (Fig. 3). As for the left eye, a visual acuity of 20/20 was observed, IOP 13, positive photomotor reflex; at the anterior capsular and subcapsular level, minimal opacities were observed. The auxiliary method of the right eye ultrasound was requested, which reported an increase in echogenicity and anteroposterior diameter of the lens, the other structures were found without valuable data.

Figure 3. Leukocoria at the level of the right eye.
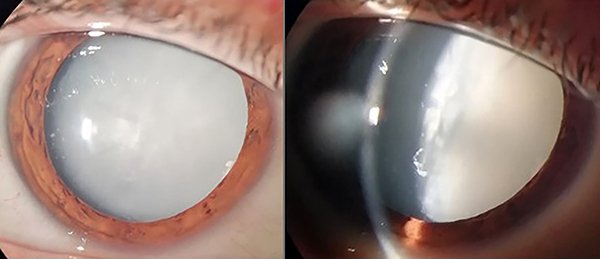
Figure 4. Biomicroscopic image of the traumatic cataract at the right eye.
Phacoemulsification was performed with trypan blue capsular staining prior to capsulorhexis and implantation of a foldable IOL in a capsular bag, without complications.
On the 5th postoperative day of the right eye, a transparent corneal, slight inflammation, IOL in the capsular bag, a 20/20 visual acuity without correction was observed.
Discussion
The formation of cataracts after various types of exposure to electricity has been reported, among which examples can be cited in electrical cardioversion, electrocution in an electric chair and in accidents due to electrical burns2-4,6-8. For unknown reasons, electroconvulsive therapy does not cause cataracts9.
The reported incidence of cataracts in patients with electrical injuries ranges from 0.7% to 8.0%2. It is assumed to be due to differences in the voltage and duration of action of the current, the distance of the eye contact area, the extent of the surface contact, and the direction the current takes in the body. It will depend on whether these factors are more focused towards the eye. The strength of the electrical current that causes cataract formation is considered to vary between 220 to 80,000 volts2,7.
The appearance of cataracts as a consequence of severe electrocution, in the Department of Ophthalmology at Yale Hospital has been reported with an incidence of up to 5% in patients with current entry points on the neck10. The exact pathogenesis of electrical cataract is controversial, and several theories have been proposed3. The characteristics of this type of cataract usually present with edema of the lens, which progresses rapidly to a mature one due to increased proliferation and rupture of lens fibers4. In relation to our case, the patient had contact through the right arm while doing gardening work and only reported progressive decrease in vision in the right eye that was accentuated 4 months after the accident.
Electrocution cataracts may manifest immediately as well as sometime later, from days to months, even years. A latency period of up to 11 years after the event has been reported2-4,11.
This type of accident or events related to electrocution should have a complete routine ophthalmology evaluation, as soon as the patient is stable. Although they turn out to be a minimal cause of frequency, you should think about the possibility of their existence. There is no large sample study, so it would be an important public health issue to consider.
In conclusion, these cases, without previous affection, are accompanied by a good state of the optic nerve as well as the retina, for which a correct diagnosis and elective surgery without complications is considered to have a good visual prognosis.
References