
CASE REPORT
Tolosa-Hunt syndrome in a young female: a case report
María Ignacia Oliva Gómez Centurión(a), Carlos Alberto Escudero(b), Guillermo Campolongo(b), Julieta Gancedo(a), Noelia Rubert(a), Leandro Emanuel Diaz Herrera(a)
a) Dra Mulet Eye Clinic, Mendoza, Argentina.
b) Spanish Hospital of Mendoza, Argentina.
Received: February 24th, 2022.
Aproved: May 3rd, 2022.
Corresponding author
Dr. Leandro Emanuel Diaz Herrera
leaadiaz@gmail.com
Oftalmol Clin Exp (ISSNe 1851-2658)
2022; 15(2): e198-e203.
Acknowledgements
We would like to thank Gochicoa Paula, MD Fellowship in Paediatric Ophthalmology & Strabismus Italian Hospital Buenos Aires and Dra Mulet Eye Clinic for her contribution in the diagnostic work-up of the patient.
Abstract
Purpose: Tolosa-Hunt syndrome (THS) is a rare steroid-responsive etiology for painful ophthalmoplegia. Our purpose is to present an interesting case of THS in a young female.
Case report: A 17 year old female consulted due to severe frontal headache and left-sided periorbital pain, with the left eyelid ptosis and diplopia. Visual acuity was 20/20 in each eye. Intraocular pressure, anterior segment and fundus examination was normal in both eyes. Ocular movement was restricted to adduction in left eye with painful movements, upper left-sided eyelid ptosis and partial left-sided oculomotor cranial nerve palsy. Laboratory tests were within normal limits and a cranial multi-slice computed tomography was reported normal. Magnetic resonance imaging was performed: the brain and the orbits are described as signal isointense on T2 weighted scans in left transverse sinus. On the basis of history and imaging, a diagnosis of THS was made and the patient was started on corticosteroid therapy (methylprednisolone, 1 g IV for 3 days), and a dramatic improvement in diplopia and pain was noted within 48 hours of starting steroid therapy. After 6 weeks of oral prednisolone a full remission of the condition was attained.
Conclusion: THS is a diagnosis which is managed and follow-up by several specializations (emergency physicians, neurologists, neurosurgeons, ophthalmologists and otolaryngologists). The data regarding the disease course and management remain scarce, thus reporting new cases are very important.
Key words: Tolosa-Hunt syndrome, painful ophthalmoplegia, corticosteroids.
Síndrome de Tolosa-Hunt en una mujer joven: reporte de caso
Resumen
Objetivo: El síndrome de Tolosa-Hunt es una rara etiología de oftalmoplejía dolorosa que responde a los esteroides. El propósito de este trabajo es presentar un interesante caso en una mujer joven.
Reporte del caso: Una mujer de 17 años consultó por cefalea frontal severa y dolor periorbitario izquierdo, con ptosis palpebral izquierda y diplopía. La agudeza visual era de 20/20 en cada ojo. La presión intraocular, el segmento anterior y el examen del fondo de ojos eran normales en ambos ojos. Los movimientos oculares eran dolorosos y la aducción del ojo izquierdo estaba restringida. Los test de laboratorio estaban dentro de límites normales y una tomografía de cráneo “multi-slice” se informó como normal. Se realizó una resonancia magnética nuclear: el cerebro y las órbitas describieron una señal isointensa en los cortes de T2 del seno transverso izquierdo. Tras tener en cuenta la historia y las imágenes del caso, se realizó el diagnóstico de Tolosa Hunt y la paciente inició tratamiento con corticoides: metilprednisolona inyectable (1 gr IV durante 3 días), obteniéndose una dramática mejoría en la diplopía y el dolor, dentro de las 48 horas de haber iniciado el tratamiento. Luego de 6 semanas de prednisolona oral se observó una remisión completa del cuadro.
Conclusión: El diagnóstico de esta patología, su manejo y su seguimiento corresponde a varias especialidades (médicos de urgencias, neurólogos, neurocirujanos, oftalmólogos y otorrinolaringólogos). Los datos sobre la evolución y el manejo de la enfermedad siguen siendo escasos, por lo que la comunicación de nuevos casos es muy importante.
Palabras clave: síndrome de Tolosa-Hunt, oftalmoplejía dolorosa, corticosteroides.
Síndrome de Tolosa-Hunt em mulher jovem: relato de caso
Resumo
Objetivo: A síndrome de Tolosa-Hunt é uma etiologia rara de oftalmoplegia dolorosa que responde a esteroides. O objetivo deste trabalho é apresentar um caso interessante em uma jovem.
Relato do caso: Mulher de 17 anos consultada por cefaleia frontal intensa e dor periorbitária esquerda, com ptose palpebral esquerda e diplopia. A acuidade visual era 20/20 em cada olho. Pressão intraocular, segmento anterior e exame de fundo de olho estavam normais em ambos os olhos. Os movimentos oculares eram dolorosos e a adução do olho esquerdo estava restrita. Os exames laboratoriais estavam dentro dos limites da normalidade e uma tomografia multislice de crânio foi relatada como normal. Foi realizada uma ressonância magnética nuclear: o cérebro e as órbitas descreveram um sinal isointenso nos cortes T2 do seio transverso esquerdo. Após levar em conta a história e imagens do caso, foi feito o diagnóstico de Tolosa Hunt e o paciente iniciou tratamento com corticosteróides: metilprednisolona injetável (1 g IV por 3 dias), obtendo uma melhora dramática da diplopia e da dor, dentro de 48 horas do início do tratamento. Após 6 semanas de prednisolona oral, observou-se remissão completa do quadro.
Conclusão: O diagnóstico desta patologia, a sua gestão e o seu seguimento correspondem a várias especialidades (médicos de urgência, neurologistas, neurocirurgiões, oftalmologistas e otorrinolaringologistas). Dados sobre a evolução e manejo da doença ainda são escassos, por isso a comunicação de novos casos é muito importante.
Palavras-chave: síndrome de Tolosa-Hunt, oftalmoplegia dolorosa, corticosteróides.
Introduction
The International Headache Society trough the 3rd edition of the International Classification of Headache Disorders (ICHD-3) in 2018 defined Tolosa-Hunt syndrome (THS) as unilateral orbital or periorbital pain associated with paresis of one or more of the IIIrd, IVthand/or VIth cranial nerves caused by a granulomatous inflammation in the cavernous sinus, superior orbital fissure or orbit1.
Diagnosis is based on specific criteria that were defined in 1988 and were revised in 2018 by the International Classification of Headache Disorders1.
Although computed tomography and magnetic resonance imaging (MRI) findings are not pathognomonic, they contribute to the diagnosis and follow-up of THS2.
Tolosa-Hunt syndrome (THS) was first described by Tolosa (1954) and Hunt (1961) and has an estimated annual incidence of one case per million in adults in United States3.
THS is an unusual pathology listed by the National Organization for Rare Disorders (NORD) as an uncommon disorder defined by severe periorbital cephalalgia accompanied with ophthalmoplegia3.
The cause of THS is still idiopathic, theories suggest THS be related to non-specific inflammation (non-granulomatous/granulomatous) in the region of the cavernous sinus and/or superior orbital fissure due to excess generation of fibroblasts and percolation of septa and wall of cavernous sinus with lymphocytes and plasma cells, this can be ascertained to constant pain, which is the early exposition of this syndrome. Other potential causes could be aneurysms, traumatic insult, or neoplasms3-5.
Careful follow-up is required to exclude other causes of painful ophthalmoplegia such as tumours, vasculitis, basal meningitis, sarcoid or diabetes mellitus1.
Treatment with glucocorticosteroids is recommended in THS although controversy exists regarding dosage, route, and length of administration2.
Case report
A 17 year old female was admitted to the Eye Trauma and Emergency Department, Dra Mulet Private Eye Clinic, due to severe frontal headache and left-sided periorbital pain, with the left eyelid ptosis and diplopia.
At admission, the patient was complaining of the left-sided supra-orbital pain that expanded into the infraorbital area. During history taking, the patient reported that she has not relevant past medical history presented.
At the current admission, the patient denied having nausea, fever, or recent head trauma. The patient denied possible allergy to medications.
On ocular examination performed at admission verified right eye visual acuity of 20/20 and left eye visual acuity of 20/20.
There were no apparent pathological changes in the anterior segment of either eye.
Intraocular pressure in the right eye was 12 mmHg and in the left eye it was 12 mmHg. Fundus examination was normal both eyes, extra ocular movement was restricted to adduction in left eye with painful movements, upper left-sided eyelid ptosis, partial left-sided oculomotor cranial nerve palsy, the other cranial nerves were normal (Figs. 1, 2).

Figure 1. Neuro-ophthalmologic examination day 1.

Figure 2. Neuro-ophthalmologic examination day 1.
All the results of routine laboratory tests were within normal limits, several other serum labs including, ANA, ANCA C, TSH, T3, T4, VDRL, were performed and were within normal limits.
ECG, X-ray chest, and ultrasound abdomen revealed no abnormal findings.
Emergency cranial multi-slice computed tomography was reported normal.
The patient was sent for an MRI examination. MRI imaging was performed on a 1.5 Toshiba Vantage Elan MR scanner no contrast medium was administered, this MRI of the brain and the orbits are described as signal isointense on T2 weighted scans in left transverse sinus (Figs. 3-5).

Figure 3. Coronal T2-weigthed MRI showing signal isointense in left transverse sinus.

Figure 4. Coronal T2-weigthed MRI showing signal isointense in left transverse sinus.
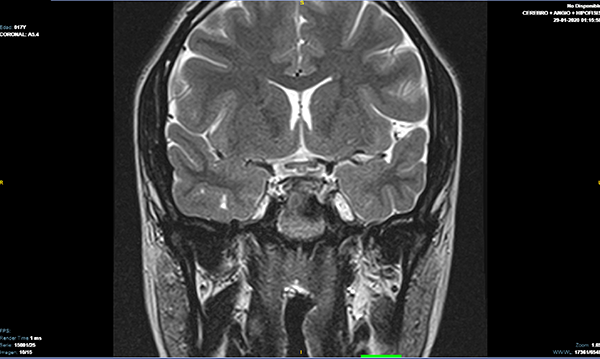
Figure 5. Coronal T2-weigthed MRI showing signal isointense in left transverse sinus.
On the basis of history and imaging, a diagnosis of THS was made and the patient was started on corticosteroid therapy: Injection methyl-prednisolone (1 g. I.V. for 3 days).
Dramatic improvement in diplopia and pain was noted within 48 hours of starting IV steroid therapy. Oral prednisolone 40 mg daily was started after 3 days and continued for 6 weeks.
Upon completion of treatment, full remission of the condition was attained, the patient was asymptomatic and her neuro-ophthalmologic examination was completely normal (Figs. 6, 7).

Figure 6. Neuro-ophthalmologic examination post steroid treatment.

Figure 7. Neuro-ophthalmologic examination post steroid treatment.
Discussion
THS is a rare cause of painful ophthalmoplegia that is caused by non specific inflammation of the cavernous sinus or superior orbital fissure of unknown etiology.
The revision of the diagnostic criteria by the ICHD in 2018 has aided the clinical diagnosis1.
Because the diagnosis of Tolosa-Hunt syndrome can been made only after other disease processes have been excluded, it is important to know the differential diagnosis of painful ophthalmoplegia, must be discarded with complementary laboratory methods and clinical and imaging improvement to corticosteroid treatment6.
Current neuroimaging modalities allow visualisation of the area of suspected pathology. Contrast enhanced MRI with multiple views, particularly coronal sections, should be the initial diagnostic study performed. Numerous reports have demonstrated an area of abnormal soft tissue in the region of the cavernous sinus in most, but not all, patients with Tolosa-Hunt syndrome6.
Typically, the abnormality is seen as an intermediate signal intensity on T1 and intermediate weighted images, consistent with an inflammatory process. In addition, there is enhancement of the abnormal area after intravenous injection of paramagnetic contrast.
Yet the signal characteristics (hypointense relative to fat and isointense with muscle on T1 weighted images; isointense with fat on T2 weighted scans) were also consistent with meningioma, lymphoma, and sarcoidosis6.
Because of this fundamental limitation of initial imaging studies, some authorities would suggest that resolution of imaging abnormalities after a course of systemic corticosteroids should be considered “diagnostic” of Tolosa-Hunt syndrome7.
Generally corticosteroid therapy such as prednisolone, methylprednisolone and dexamethasone, given either orally or intravenously for THS results in climactic improvement in pain which is usually apparent in a few days, notwithstanding the fact that corticosteroids are the cornerstone of treatment for THS, there are controversies concerning effective course, route of administration, optimal dosage, period of therapy and treatment in special groups such as pregnant women and children8.
Conclusion
THS is a diagnosis which is managed and follow-up by several specializations (emergency physicians, neurologists, neurosurgeons, ophthalmologists and otolaryngologists).
Resolution of MRI findings after a course of steroid is considered diagnostic.
Although the pathogenetic basis of Tolosa-Hunt syndrome remains unknown, from a practical clinical standpoint it can be regarded as a distinct entity which may be simulated by various other disorders.
However, the data regarding the disease course and management remain scarce, thus reporting new cases are very important.
It is also important to continue with controls every 6 months to evaluate evolution.
References